2021 - Multiple Choice Questions
Which drug increases uterine tone
- Ergometrine
- Magnesium
- Salbutamol
- GTN
How does hyperkalemia affect the action potential
- Increases the resting membrane potential
- Increase in slope of phase 2
- Increase in threshold potential
- Increased velocity of phase 0
- Decreased RMP
- Velocity (Vmax) of Ph 0 decreases as RMP becomes less negative
- Threshold potential decreases (from -75mV to -70mV)
- Increase in slope of Ph 2 & 3 shortening repolarisation time (responsible for ST-T depression, peaked Tw & QT shortening)
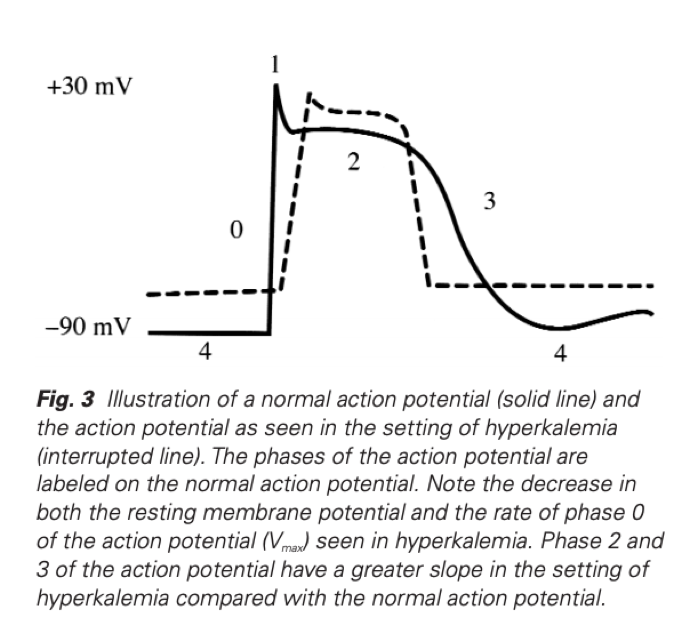 Hyperkalaemia Revisited, Parham W et al, Tex Heart Inst J 2006;33:40-7
Hyperkalaemia Revisited, Parham W et al, Tex Heart Inst J 2006;33:40-7 The position with the greatest reduction in FRC:
- Supine
- Trendelenburg
- Erect
- Prone
The correct order of the ECG and CVP trace on Wigger’s diagram:
- C wave R wave T wave V wave
- R wave C wave V wave T wave
- C wave R wave T wave V wave
- R wave C wave T wave V wave

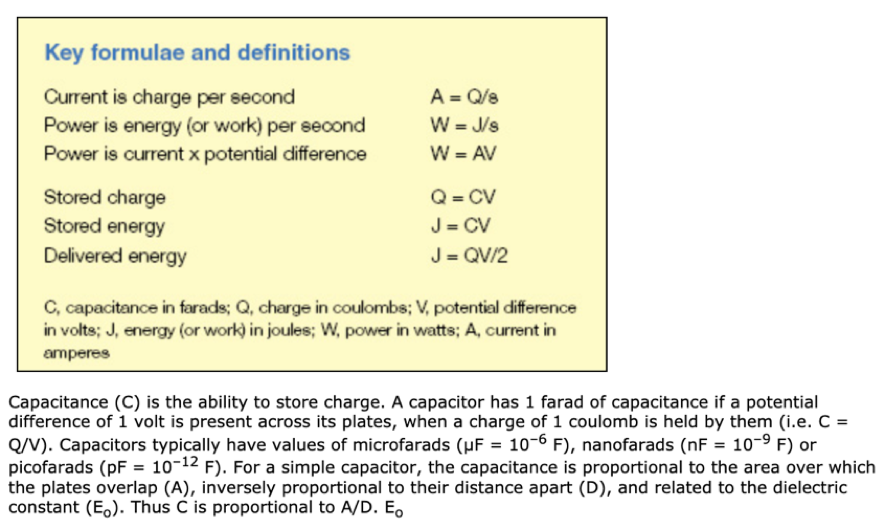
Capacitance is measured in
- Volts
- Watts
- Farads
- Joules
This qn was recalled as something in regards to a defibrillator capacitance refers to…
Capacitance is the ability to store charge (SI = Farad)
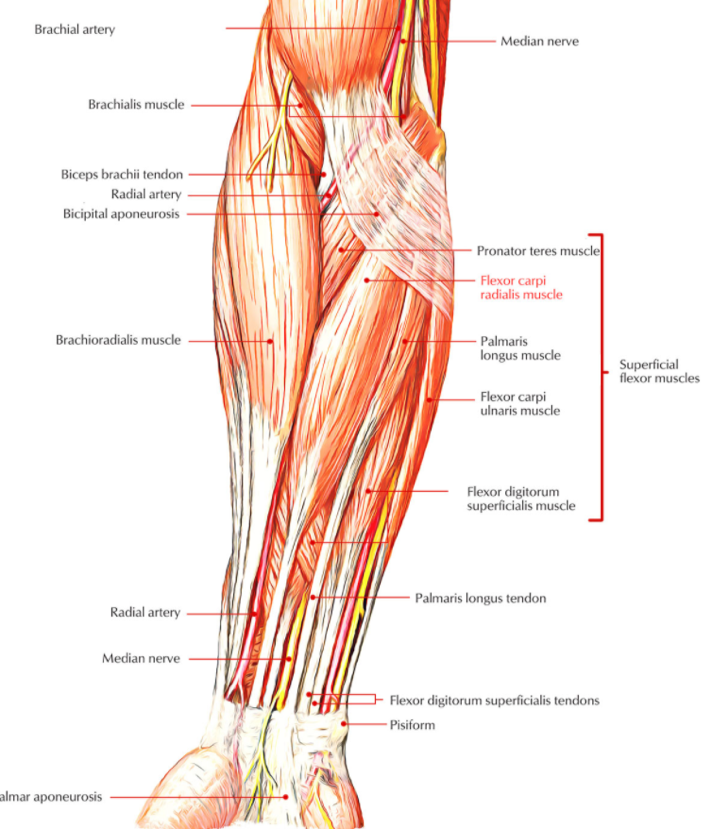
The correct surface anatomy of the radial artery in the distal forearm
- Medial to the Median nerve
- Lateral to the flexor carpi radialis
- Medial to the Ulnar nerve
- Lateral to the brachioradialis
The most lateral structure:
- Femoral Artery
- Femoral Vein
- Femoral Nerve
- Femoral Canal
Too easy.
They could potentially confuse by asking you the most lateral structure in the femoral sheath (as opposed to the triangle which does not contain the nerve)
The events occurring in Phase II of the Valsalva Manoeuvre:
- ↓BP, ↑HR, ↑Intrathoracic Pressure
- ↑BP, ↓HR, ↑Intrathoracic Pressure
- ↓BP, ↑HR, ↓Intrathoracic Pressure
- ↑BP, ↓HR, ↓Intrathoracic Pressure
An additional variable added to the 2019 MCQ


Permanent closure of Ductus Arteriosus after birth occurs
- 1-5 mins
- 1-5 hours
- 2-3 days
- 2-3 weeks
The ductus arteriosus is a fetal vessel that allows the oxygenated blood from the placenta to bypass the fetal lungs in utero. At birth, a newborn inhales for the first time and the lungs fill with air, causing pulmonary vascular resistance to drop and blood to flow from the right ventricle to the lungs where it can undergo oxygenation. The increased arterial oxygen tension and decrease in blood flow through the ductus arteriosus causes the ductus to constrict and functionally close by 12 to 24 hours of age in healthy, full-term newborns, with permanent (anatomic) closure occurring within 2 to 3 weeks. In premature infants, the ductus arteriosus does not close rapidly and may require pharmacologic or surgical closure to treat unwanted repercussions
- Patent Ductus Arteriosus
- Maria Gillam-Krakauer; Kunal Mahajan.
The S wave of the ECG occurs:
- After blood is ejected into aorta
- After the fourth heart sound
- During isovolumetric contraction
- Preceeding the ‘a’ wave

Which is true of anatomy of the Radial Artery:
- Splits into thenar and hypothenar arteries
- Lateral to flexor carpi radialis
- Medial to palmaris longus tendon
- Deep to medial nerve under flexor retinaculum
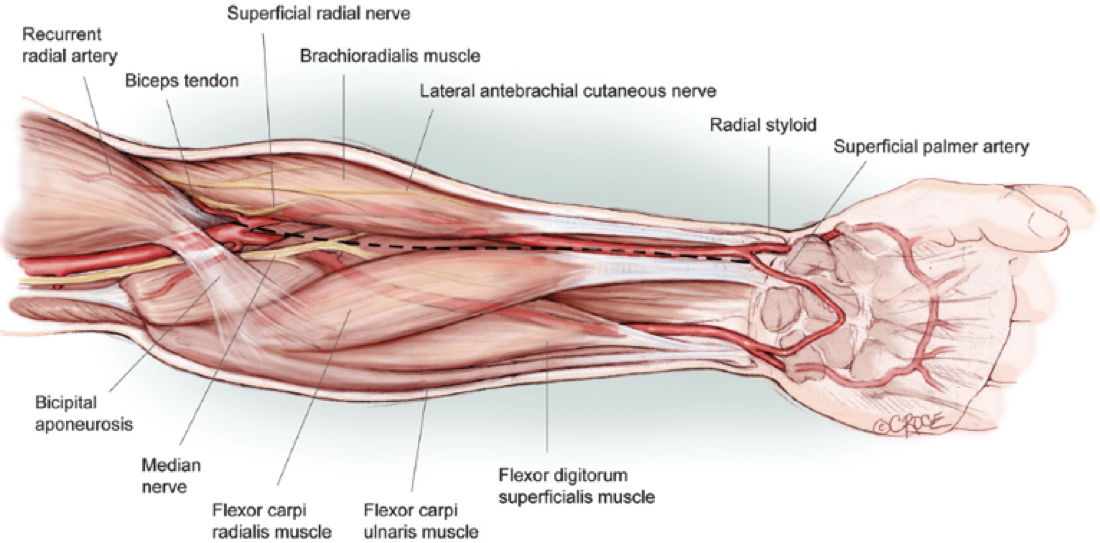 Harvesting the Radial Artery
Arie Blitz et al
Harvesting the Radial Artery
Arie Blitz et al Oxygen tension in the blood measured by:
- Absorbance spectrophotometry
- Paramagnetic analysis
- Pulse contour analysis
- Mass spectroscopy
Paramagnetic Oxygen Analyser
Clarke Electrode
Which phase of the cardiac cycle has the highest sodium flux:
- Isovolumetric Contraction
- Isovolumetric Relaxation
- Ejection
- Atrial Systole A)
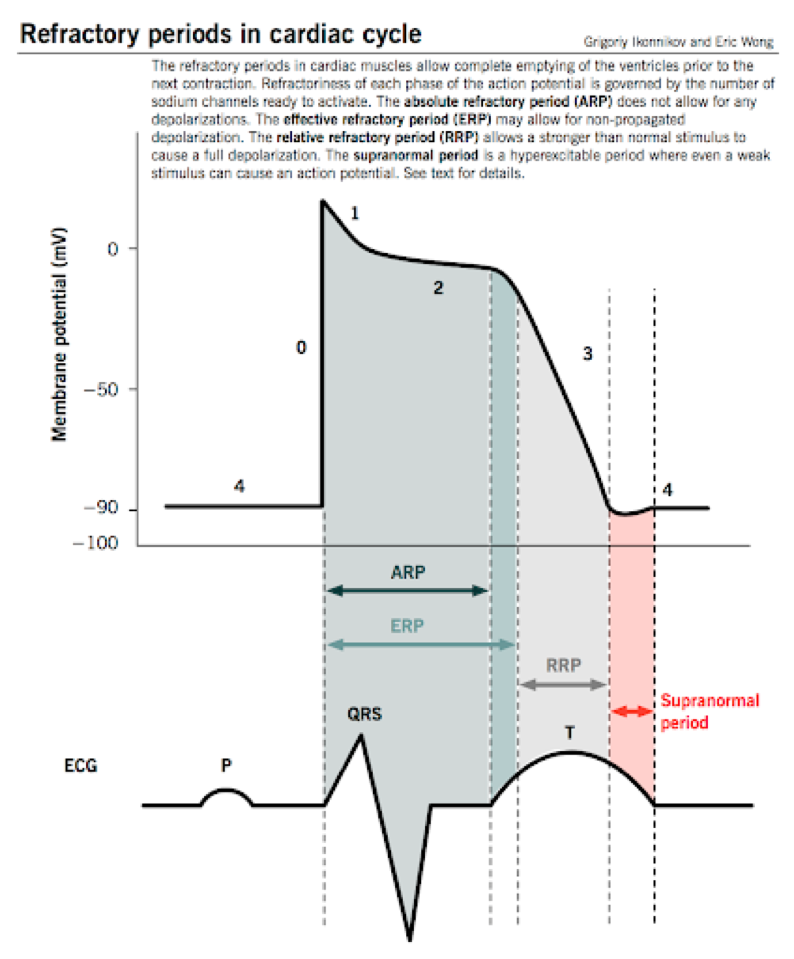 Isovolumetric ventricular contraction
Isovolumetric ventricular contraction
- The beginning of this phase corresponds with the peak of the R wave
- This corresponds to Phase 0 (rapid sodium influx) of the ventricular myocyte action potential
- The ventricles begin to contract during this period
- This contraction increases the ventricular chamber pressure and closes the mitral and tricuspid valves.
- As a result, there is a fixed ventricular volume during this contraction
The drug with the lowest clearance:
- Vancomycin
- Piperacillin-Tazobactam
- Clindamycin
- Ampicillin
The nerve root of the knee jerk reflex
- L1/L2
- L3/L4
- L4/L5
- S1/S2
Just be sure you are answering the correct qn as there are Dermatome, Myotome & Reflex MCQs
The efferent limb of the pupillary light reflex synapses onto post-ganglionic parasympathetic fibres in the:
- Olivary Pretectal Nucleus
- Edinger Westphal nucleus
- Ciliary Ganglion
- Contralateral Pretectal Nucleus
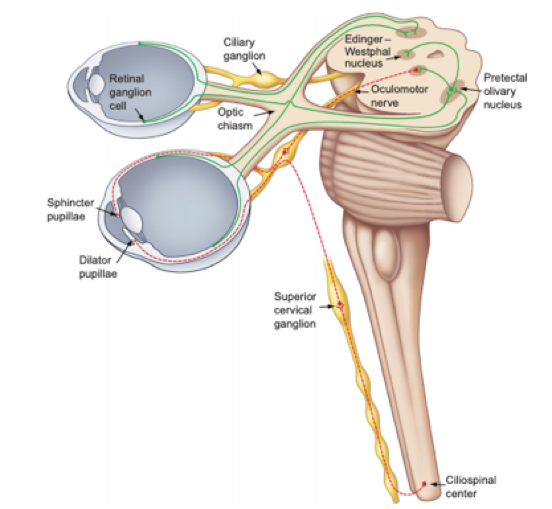
This qn was not well recalled but related to the pupillary light reflex – learn the pathways & their connections
- The PLR has traditionally been divided into two separate pathways based on the clinical manifestations of the defects in this reflex.
- The afferent pathway is composed of both the retinal cells that project to the pretectum as well as their recipient neurons, which project bilaterally to the EW nucleus (Figure 1).
- The efferent pathway is composed of the preganglionic pupilloconstriction fibers of the EW nucleus and their postganglionic recipient neurons in the ciliary ganglion, which project to the sphincter muscle of the iris (Figure 1).
The effect of a competitive antagonist on a dose response curve is:
- Right shift
- Change in slope
- Change in peak
- Left shift
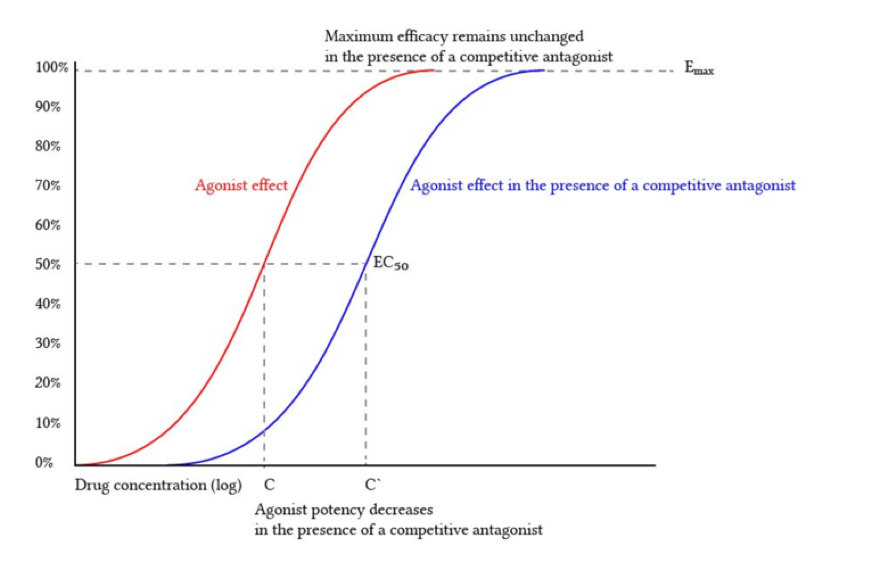 Deranged Physiology
Deranged Physiology Drugs with low extraction ratio are primarily affected by
- Hepatic blood flow and intrinsic enzyme activity
- Hepatic blood flow and plasma protein binding
- Protein binding and intrinsic enzyme activity
- Hepatic blood flow only
For drugs with low extraction ratio:
- only unbound drug penetrates membranes and is available for elimination. An increase of the unbound fraction will thus proportionally increase the clearance
- Variation of the organ’s intrinsic ability to eliminate the drug will also slightly affect organ clearance
Which is true regarding the antifungal activity of anidulafungin:
- Inhibits glucan synthase
- Inhibits ergosterol synthesis
- Narrow spectrum limited to yeast organisms
- Is affected by renal impairment
- Anidulafungin has potent and broad antifungal activity against Candida and Aspergillus spp., including those resistant to fluconazole
- It does not undergo metabolism but is eliminated through spontaneous degradation with linear kinetics and a terminal half-life of 40 to 50 hours
- Neither end-stage renal impairment nor dialysis substantially alters the pharmacokinetics of anidulafungin.
GFR can be directly measured through
- Creatinine Clearance
- Para-aminohippurate clearance
- Lithium Clearance
- Inulin Clearance
- Crt & Cystatin both indirect measurements
- PAH is for RBF
- Lithium for proximal fluid reabsorption