Digoxin
Chemical
A cardiac glycoside naturally occurring in many plants
- Basic structure → steroid nucleus with a glycose & aglycone portion
Glycose → glucose → required to fixate the glycoside to cardiac muscle
Aglycone → influences PD effects
Use
- Treatment of heart failure
- Slow ventricular response rate
Dose
Load: IV 0.5mg/30mins or 10mcg/kg
Maintenance: 0.125 – 1mg/day
Route
PO/IV
Onset
IV: 15 mins
PO: 1 – 6hrs
DoA
Several days
t ½ 40hrs with normal renal function
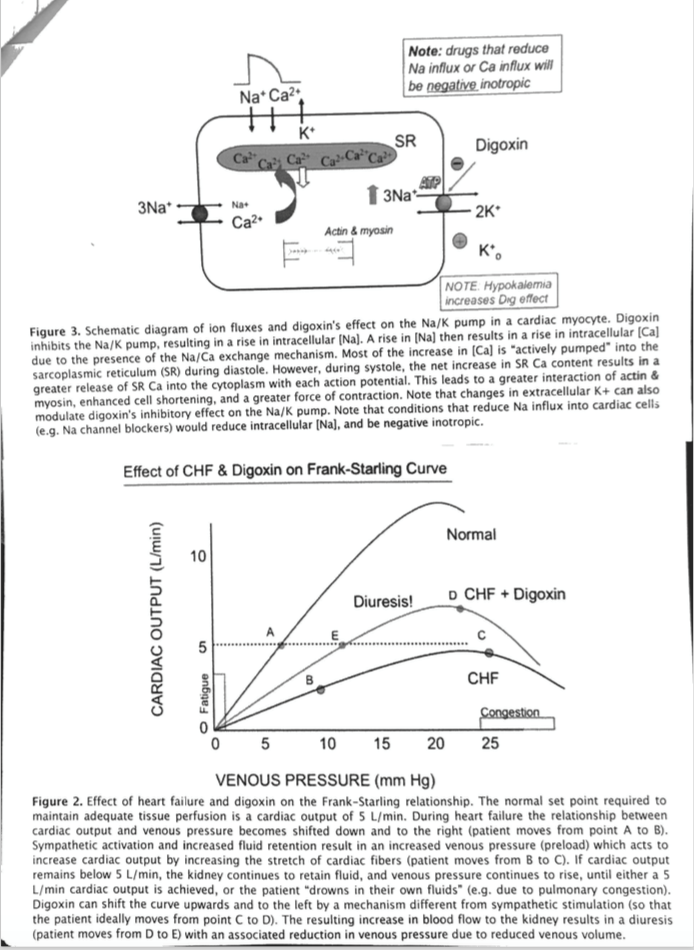
MoA
Peripheral vascular effect
Myocardial → DIRECT → MECHANICAL
- Inhibits Na/K/ATPase (binds directly)
- ↑intrac. Na+
- ↓activity of Na+/Ca2+ exchanger
- ↑intrac. Ca2+
- Causes further release of Ca2+ from SR = ↑force of contraction
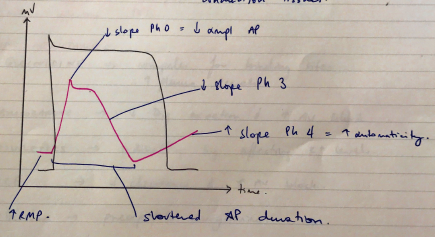
Myocardial → DIRECT → ELECTRICAL
- Inhibits Na/K/ATPase
- Which is essential for maintaining normal RMP/ion concentration
= ↑automaticity
- RMP becomes less negative (depol easier) 2° ↑intrac. K
- AP shortens 2° ↑K conductance
- ↑slope of Ph 4
- ↓slope Ph 0 because less Na gradient (this is the only ∆ that doesn’t ↑automaticity)
Myocardial → INDIRECT → ↑PARASYMP ACTIVITY
- Sensitizes CAROTID SINUS BARORECEPTORS
- Activates vagal nuclei
- Facilitates muscarinic transmission at cardiac cell
→ CHOLINERGIC INNERVATION MORE PRONOUNCED IN ATRIA →
∴ affect atria & AV node movement
- – VE CHRONO / -VE DROMO
Peripheral vascular effects
- Inhibition of Na/K/ATPase of vascular sm m → depolarization → smooth muscle contraction → VC → = ↑PreL & SVR
ECG Effects
ECG ∆
Prolonged PR
Mechanism
Delayed AV conduction
ECG ∆
Scooped out ST
Mechanism
↓slope Ph 3 due to ↑K conductance
ECG ∆
T waves ↓amplitude ST inversion
Mechanism
ECG ∆
Shortened QT
Mechanism
↑K conductance, shortens AP
ECG ∆
NO EFFECT QRS DURATION
Mechanism
Because digoxin doesn’t alter conduction through ventricles or conduction tissues
PD
CVS
- ↑myocardial contractility
- ↓HR
- ↑SVR
RENAL: ↑renal perfusion & mild diuresis
Response Variability
Elderly: ↓skeletal m. = ↓reservoir = ↑plasma levels
Renal failure: ↓dose
Ab development: ↓therapeutic effect
Drug Interactions
- Factors affecting absorption
- Factors affecting PPB
ANTIARRHYTHMICS
- Quinidine → competes for binding sites ∴↑plasma levels
- Amiodarone → ↓dig excretion & ↑AV block
- Diuretics → Indirectly by affecting K+ levels
- CCB → ↓clearance & ↑AV block
- Β-blockers → precipitate arrhythmias
- Potassium → & dig inhibit each other binding to Na/K/ATPase
- ↑K = ↓effect on Na/K/ATPase
- ↓K = ↑effect on Na/K/ATPase
- Calcium → overloads Ca2+ stores = ↑automaticity ∴↑risk arrhythmias
- Magnesium → opposite effect to Ca2+
- Erythromycin → ↑GI absorption (unpredictable, not all patients)
PK
A
75% OBA
Peak plasma in 1 – 2hr
D
PPB 25%
VD 6L/kg
Tissue affinities:
- Heart → 15 – 30x plasma levels
- Skeletal m. → 50% less cardiac levels
→ Principle reservoir
- Fat → minimal accumulation
M
Minimal
E
Excreted by kidneys unchanged
Depends on CrCl
t ½ B = 2 days!
NOT REMOVED BY DIALYSIS
Adverse Effects
[Digoxin] myocardium = much more than plasma
Monitor levels
→ 6 – 12hr post dose
→ 0.6 – 2.6nmol/L
But relationship between level & pharmacological effect not always consistent
→ <0.5nmol/L = no dig toxicity
→ >3nmol/L = definitely toxic
TOXIC EFFECTS → Na/K/ATPase inhibition
CVS
- Heart block (AV conduction delayed)
- Arrhythmias (↑slop 4, ↑Ca2+ intrac) → any arrythmia but VF most common cause of death from dig toxicity
CNS
- Insomnia
- Agitation
- Confusion
- Delirium
- Xanthopsia (seeing yellow)
GI: anorexia, N&V (stimulations CTZ)
RISK FACTORS:
- Renal impairment
- Elderly
- ↓K
- ↑Ca2+
- ↓Mg2+
Tx:
- Stop drug
- Tx arrhythmia
- Replace electrolytes
- Consider DIGOXIN SPECIFIC AB’s
→ Bind dig ∴ less available to inhibit Na/K/ATPase
→ Dig-Ab complex eliminated by kidneys