23A08: Exam Report
Describe the cardiovascular and respiratory effects of positive pressure ventilation
21% of candidates passed this question.
This question required a breadth of response that was largely unrepresented in the answers provided by candidates.
Better answers divided responses into cardiovascular effects and respiratory effects however many did not provide sufficient detail or provided only detail on some of the effects and missed the breadth of the question.
Cardiovascular effects could be grouped into effects on the; right heart, left heart, ventricular interdependence, cardiac output, other circulations, baroreceptor and hormonal reflexes.
Respiratory effects could be grouped into lung volumes, dead space, V/Q matching, compliance, airway resistance and the effect of excessive pressures on the lung.
Despite this division in the question many candidates abandoned a structure which made their answers and explanations lack clarity.
The examiners commented that most candidates who wrote an answer in paragraph format were likely to provide long vague answers rather than those more factual and succinct answers presented in a format with headings as above and pertinent associated dot point descriptions underneath these headings.
F10i / 23A08: Describe the cardiovascular and respiratory effects of positive pressure ventilation
Respiratory Consequences
Positive pressure ventilation (PPV) is the delivery of gas through positive pressure by a machine either non-invasively through a mask or invasively through an ETT/tracheostomy
SPV
- INSP: small negative intrapleural, interstitial and alveolar pressures generated allowing lung to inflate
- EXPR: intrapleural pressure returns to atmosphere but remains negative
PPV
- INSP: high intrathoracic pressures transmitted to alveoli & interstitial tissues to inflate alveoli
- EXPR: return to atmosphere (but if PEEP is added will remain positive)
PPV heart-lung interactions
- PPV increases Intrapleural pressure and intrathoracic pressure
- This pressure is applied to all intrathoracic structures – including the heart
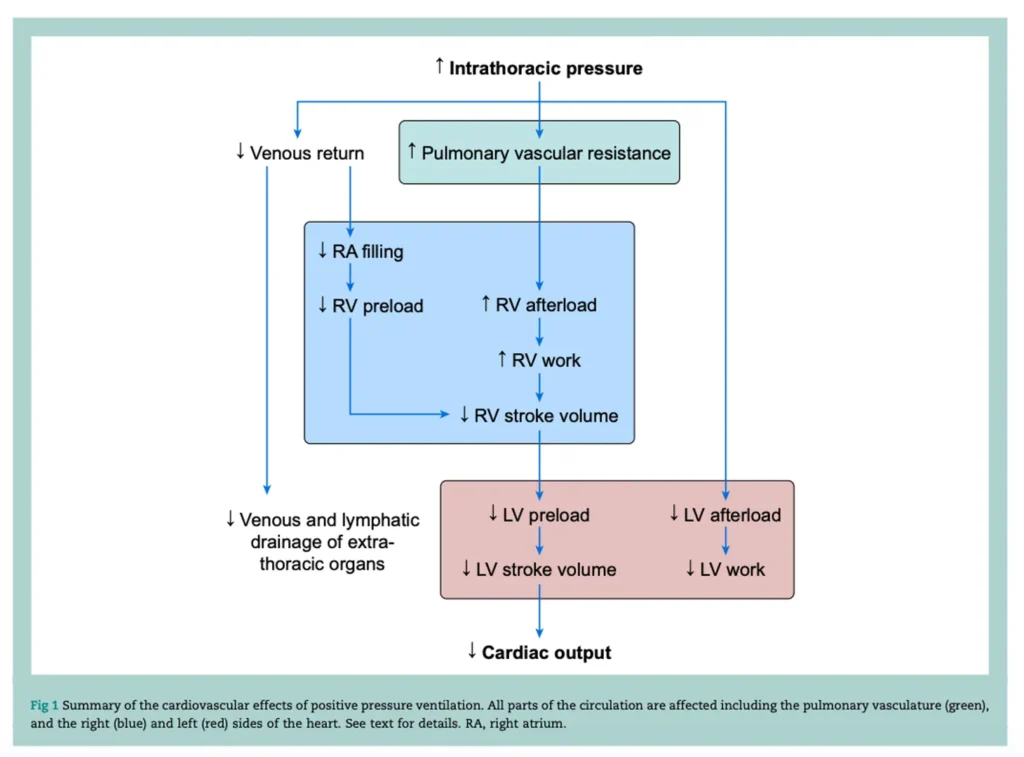
- (BJA Education, 21 (6): 202-209 (2021) – The Cardiovascular effects of PPV)
CARDIOVASCULAR
R) Heart
- Increase in RA pressure
- Reduces venous return
- Reduced RV preload
- Increase in RV afterload
L) Heart
- Increased intrathoracic pressure
- Reduces transmural P of LV
- Increases wall tension by Law of LaPlace
- Reduces LV afterL
- But the reduction in LV filling dominates so even though there is a reduced LV afterload there is still a reduction in LV CO
- Reduction in LV afterload
- Reduced myocardial O2 demand
Cardiac Output
- Reduces LV preload due to lower RV output
- Reduces LV stroke volume
- Reduced CO
Pulmonary Blood Flow & Ventricular Interdependence
- Increased airway pressure and application of PEEP and the effect on PVR depends on whether alveoli are recruited to FRC or overdistended
- Overdistention increases PVR and reduces pulmonary blood flow
- Expansion of lungs units to FRC reduces hypoxic vasoconstriction and PVR therefore facilitating pulmonary blood flow
- Increase in RV afterL
- Bulging of IV septum into LV
- Reduce LV compliance and LV filling
- Reduced CO
Other Circulations
- IVC – reduction in diameter
- Lymphatic Circulation – reduction in flow and interstitial fluid retention owing to loss of negative intrathoracic pressure which drains the lymphatic system, collapse of thin-walled lymphatic vessels and an increase in central venous pressure
- Renal perfusion & Glomerular filtration – reduced and increase in ADH
- Hepatosplanchnic perfusion – reduced
- ICP / Cerebral Perfusion – affected by PPV owing to reduction in MAP
Baroreceptor
- Increase in pleural pressure
- Increases aortic pressure
- Triggers peripheral baroreceptors
- Lowers SVR and LV afterload
- Reduction in CO
Hormonal Reflexes
- Reduction in LA stretch receptors due to reduced preL
- Increase in ADH and ANP
- Increase H20 absorption
RESPIRATORY
Lung Volumes
- PEEP = increase FRC
Dead Space
- NIV increases anatomical dead space
- ETT reduces anatomical dead space
- Physiological dead space depends on pathology
V / Q Matching
- Increasing PEEP increases alveolar recruitment
- Reverses hypoxic vasoconstriction
- Improves V/Q matching
- Improves oxygenation
Compliance
- Determined by compliance of lungs & chest wall
- Optimal compliance will be at optimal PEEP
- Optimal PEEP = that which results in the lowest driving pressure (Pplat-PEEP)
- PEEP associated with maximal alveolar recruitment will give the best compliance, however with over distention, compliance decreases and Pplat will rise
- PPV preferentially aerates high compliance areas
Airway Resistance
- Tissue & Airway resistance
- Tissue = friction caused by moving organs and chest wall
- Airway (RAW) = friction caused by air moving through respiratory system and conducting airways
- RAW in SPV is 0.6-2.4cm H20/L/sec
- RAW MV is 5-10cm H20/L/sec
- High risk of higher RAW due to secretions, bronchospasm, ETT compression, mucus plugging and high airflow rates predisposing to turbulent flow
Work of Breathing
- Aims to reduce either partially or completely depending on the mode of PPV
Surfactant
- Asymmetrical spread of surfactant across alveoli
- Altered production of surfactant (loss of T2 pneumocytes)
- Overall changes in surface tension and loss of immunocompetence & increasing the risk of further injury
Excessive pressures on the lung
- Induce / worsen lung injury (VILI)