F6v: Explain the concept of shunt, its physiological effects, and its measurement
Definition
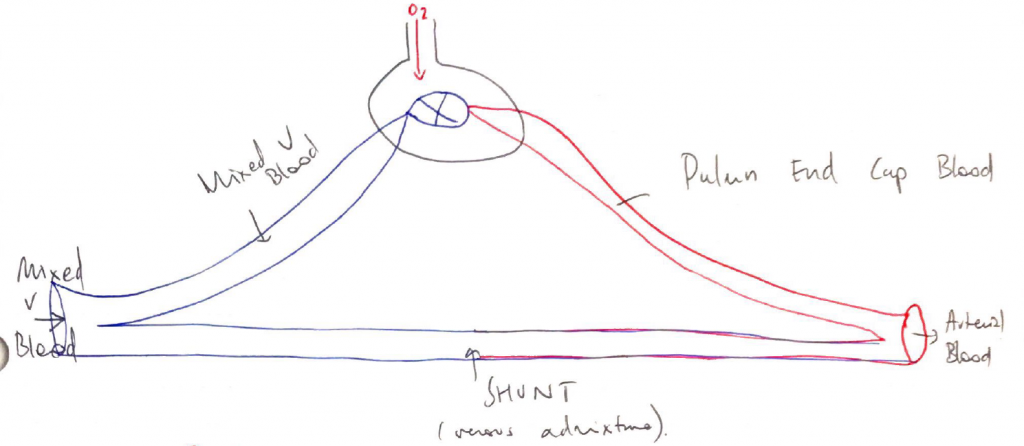
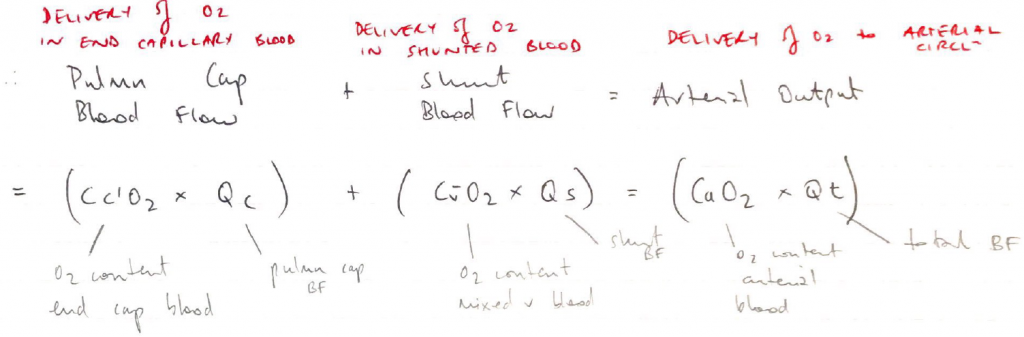
- Shunt = blood that enters arterial circulation without passing through ventilated lung
Causes of Shunt
Physiological
- Bronchial circulation → adds deoxygenated blood to pulm v (not mixed venous blood)
- Thebesian veins → empty directly into LV cavity (also not true mixed venous blood)
Pathological
- Non-ventilated alveoli → V/Q = 0 (true mixed venous blood)
- Cardiac defects → R – L shunt (true mixed venous blood)
NOTE: Although bronchial & thebesian veins do not contain true mixed venous blood (&∴ strictly can’t be calculate with SHUNT EQUATION), we do use shunt equation to quantify them
Effect of Shunt on PO2
- Shunt ↓O2 content of arterial blood
- This does not respond to ↑FiO2
- Because no matter how much ↑FiO2 you give, the shunted blood is never exposed to it
- ∴giving 100% FiO2 is a useful diagnostic test → there’s a huge A – a gradient
- The larger the shunt, the smaller the ↑PaO2 for given ↑FiO2
- Sigmoid ODC:
- Blood passing past high FiO2 units is already fully saturated its Hb, so any additional O2 is only dissolved, which is small
- Blood coming out of these units is not enough to close the shunt gap
Effect of Shunt on PCO2
- Shunted blood does not ↑PaCO2
- 2 reasons:
- CO2 curve is linear → regardless if PO2 is high/low
- Respiratory compensation
- Any ↑PaCO2 stimulates chemoR → ↑MV
- Keeps PaCO2 normal range
- This ↑MV does not connect hypoxaemia
- But hypoxaemia can ↑MV further (so PaCO2 may even be low)
HALLMARK of SHUNT → ↓PaO2 + low/normal PaCO2