H1ii: Physiological factors that determine oxygen delivery to the renal medulla
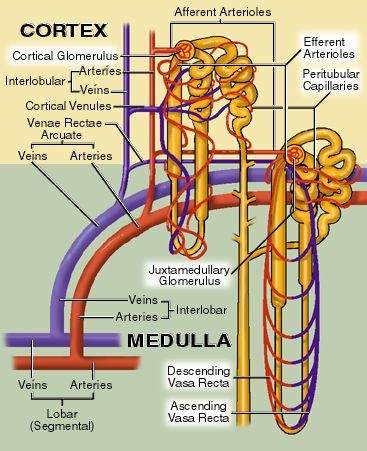
Renal Vascular Anatomy
- No glomeruli exist in renal medulla
- Efferent arterioles of deep (juxtaglomerular) nephrons descend down to medulla + form VASA RECTA
Efferent arteriole
↓
Descending vasa recta
↓
Ascending vasa recta
↓
Veins
- Vasa recta have different structure along their tracts
- Desc = arteriole like
- Loop = capillary like
- Asc = fenestrated endothelium to allow solute exchange
Renal Blood Flow
- RBF = 20% CO
= 1.2L/min
= 600mL/kidney/minute
- But RBF is not evenly distributed
- 90%
- Cortex
- Flow dependent function
- Glomerular filtration & reabsorption
- 5mL/g/min
- PaO2 = 50mmHg
- 10%
- Medulla
- Urine [ ]
- Outer medulla = 1mL/g/min
- Inner medulla = 0.2mL/g/min
- PaO2 8 – 15mmHg (only just meets its E requirements!)
- ∴even though the medulla is more metabolically active & extremely vulnerable to hypoxic injury, it has less BF which is prioritised to cortex to allow adequate GFR
- Most tubular O2 consumption is to reabsorb Na+
- And most tissues ↑BF in response to ↑demand
- BUT ↑RBF = ↑GFR = ↑Na+ load = ↑workload & O2 requirements
- BF to medulla is v. close to its O2 requirements & pO2 of medulla much lower than Renal A
- Key role of medulla Thick Asc. LoH = active transport of NaCl = high E consumption
- So to concentrate our urine we force medullary hypoxia
- Medulla tubular cells use glycolysis (minimal E consumption) & a Na/K/2Cl co-transporter to minimise O2 requirements
- But this constant risk of hypoxia requires internal regulation for protection
- 90%
Determinants of O2 Delivery To Kidneys
DO2 = CaO2 x CO
O2 delivery = O2 constant of blood x CO
CaO2 = (([Hb] x 1.34 x SpO2) + (0.003 x PO2)
CO = HR x SV
- ∴factors affecting CaO2 & CO will affect how much O2 is delivered to kidneys
CaO2
[Hb]
Saturation of Hb
pO2 of blood
CO
HR
Preload
Afterload
Contractility
Autoregulation
- Definition = the intrinsic ability of an organ to maintain a constant BF despite changes in perfusion pressure → in kidneys, autoregulation RBF b/w MAP 95 – 170 mmHg
- 2 mechanisms of autoregulation of RBF:
- MYOGENIC → responds to ∆ arterial P
- TUBULOGLOMERULAR FEEDBACK → responds to ∆ [NaCl] of tubule fluid
Sympathetic Nerves
- Aff. & Eff. Arterioles innervated by symp n’s
- Basal symp tone is minimal
- ↓ECFV = symp. release of NA + Adrenaline → as receptor stimulation of aff. arterioles = ↓GFR/RBF
Vasoactive Hormones
VC
AII
Renin
Endothelin
Adenosine
VD
Prostaglandin
NO
ANP/BNP
Bradykinin
Factors Affecting Blood Flow to Medulla
- BF to juxtamedullary nephrons is NOT autoregulated (KAM 228pp)
- ∴influenced by symp stimulation & vasoactive factors
- Also ↓BGL & high protein meal = ↑medullary BF