H1v: The role of urea in the body
- Urea = the end product of protein catabolism. Normal urea plasma levels:
- 7 – 20mg/dL
- 3 – 9mmol/L
- 90% of nitrogen from protein catabolism enters the UREA CYCLE
Urea Cycle → occurs in liver + kidneys
2NH4+ + CO2 ⮂ UREA + 2H+ + H2O
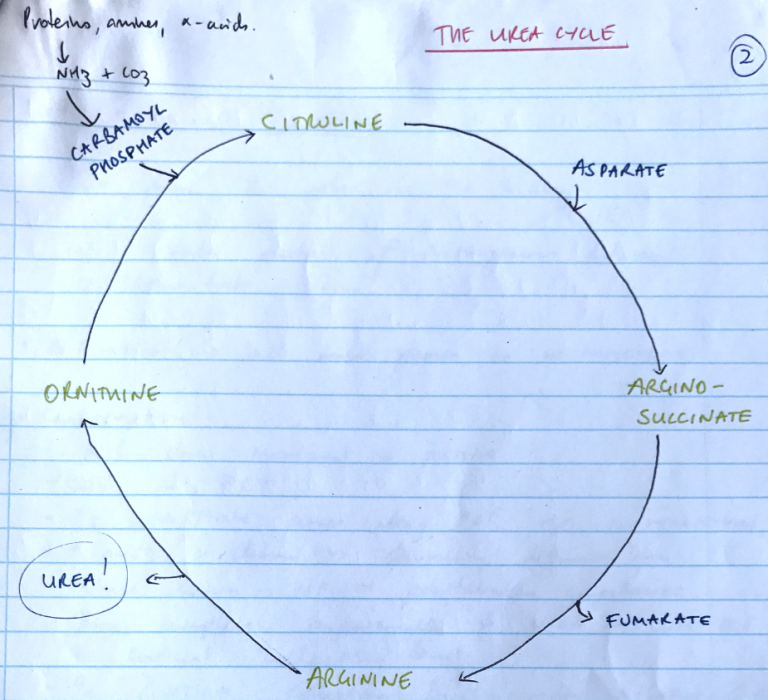
- Formation of CARBAMOYL PHOSPHATE from Ammonia + HCO3
- Condensation of carbamoyl phosphate with ORNITHINE → CITRULLINE
- Citrulline condenses with ASPARTATE → ARGINOSUCCINATE
- Arginosuccinate is hydrolysed to form FUMARATE + ARGININE
- ARGININE is cleaved → UREA + ORNITHINE
- ORNITHINE re-enters mitochondria & is combined with new CARBAMOYL PHOSPHATE to form CITRULLINE
Renal Handling of Urea
- Urea has 2 roles in the kidney
- Excrete product of nitrogenous waste
- Concentrate urine
Filtration → all urea passes to ULTRAFILTRATE
Reabsorption
- All urea movement is passive
- 50% in PCT
- As ultrafiltrate passes long PCT, H2O is reabsorbed, ↑[urea] in lumen → favouring diffusion from tubule lumen → ISF → peritubular capillaries
- Then completely impermeable to UREA in LoH, DCT & cortical collecting duct
- In CORTICAL collecting duct under influence of ADH –. Further 10% urea reabsorbed via facilitated diffusion (urea transporters which are ADH dependent)
NB: Urea reabsorption is completely dependent on H2O reabsorption
Urinary Concentration
- Urea is responsible for 50% of medullary ISF hyperosmolarity
- Because there is no urea reabsorption after PCT → medullary CD
- There is a v. high [urea] medullary CD & when urea transporters are inserted under influence of ADH, there’s a huge [ ] grad to drive it into Medullary ISF
- There it promotes even more H2O reabsorption to create a concentrated urine