H3i: List the classes of drugs that are useful in inducing diuresis & outline their mechanism of action
- Diuresis = ↑Na+ & H2O loss from the kidneys
- 1° aim of drug diuresis is to ↑Na+ excretion (KA NATRIURESIS) to ↓ECF volume
Factors Affecting Diuretics
- To work, a diuretic must reach its SoA
- Most work on nephron lumen
- Aldosterone works intracellularly
- CA Inhibitors work on lumen & intracellularly
- Diuretics gain access via GF
- Some have large PPB (i.e. frusemide)
- ∴effect of diuretic will be blunted with ↓GFR, ↓PPB, or by other drugs competing for binding
Diuretics Grouped Based on SoA
- PCT: osmotic diuretics, carbonic anhydrase inhibitors
- Ascending LoH: loop diuretics
- Distal tubule: thiazides
- Collecting duct: K-sparing diuretics, aquaretics
Osmotic Diuretics
- Small molecular weight substances
- Freely filtered at glomerulus
- Not/minimally reabsorbed
- Do not act on a membrane protein
- Simply exert an osmotic force
- 65% Na+ & H2O reabsorbed @ PCT → ∴need to act here to score $$$
- The osmotic force inhibits fluid reabsorption
- Causes some Na+ loss
- But the Na+ can be reabsorbed downstream @ thick asc. LoH
- Natriuresis only 10% of filtered load (because acts so early)
- In disease: glucose
- Therapeutics: mannitol
Also
- Impairs H2O reabsorption of Thin Desc. LoH because dissipates ISF osmotic gradient
- ↑RBF
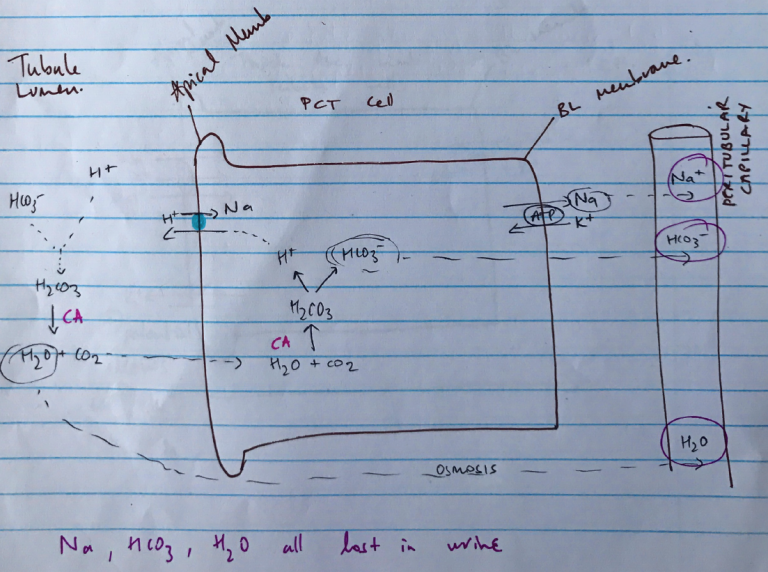
Carbonic Anhydrase Inhibitors
- Enzyme CA present in PCT (heaps), Thick Asc. LoH & Intercalated cells of Collecting Duct
- Present in tubule lumen & tubule cells
Drives equation: H+ + HCO3– ⮂ H2CO3 ⮂ H2O + CO2
- Non-competitive inhibition of CA by acetazolamide blocks NaHCO3 reabsorption by:
- ↓H+ supply in tubule cell
- H/Na antiporter can’t work
- Na+ is not reabsorbed, H2O follows
- 1/3 Na+ reabsorbed by Na/H antiporter
- Modest diuresis
- NaHCO3 loss creates alkaline urine & metabolic acidosis in plasma
Loop Diuretics
- Most efficacious diuretics
- Inhibit Na/K/2Cl symporter on Thick Asc. LoH
- ↓Na & H2O reabsorption
- 25% Na+ reabsorbed at Thick Asc. LoH
- & responsible for counter-current multiplication
- ∴kidney loses huge Na+ load & ability to concentrate urine
- Occurs late in nephron ∴limited ability to reabsorbed Na+ later
Also
- ↑RBF
- Loss of +ve potential from K+ recycling which aids Mg2+/Ca2+ reabsorption = Mg2+/Ca2+ loss
K+ Sparing Diuretics
- Act at late DCT & collecting duct (because this is where K+ secretion occurs)
- 2 types:
- SPIRO → antagonises aldosterone
- AMILORIDE → blocks Na+ entry on Apical Na+ channel
Principle Cells
Spironolactone
- Synthetic steroid
- Competitive antagonist of aldosterone
- Binds aldosterone receptor → inactivates
- Prevents translocation of receptor & binding to DNA
- ∴
- 1) Failure to synthesise proteins which stimulate Na/K/ATPase pump
- 2) Upregulate apical Na+ channel
- ↓Na+ reabsorption & stops K/H+ secretion
Aquaretics
- Antagonist V2 receptors on BL membrane
- Inhibit action of ADH
- Stops H2O reabsorption at collecting duct
Helpful to treat patient with hypo-osmotic ECF due to failure to excrete solute free H2O because ↑ADH from non-osmotic/non-haemodynamic mechanism (i.e. SIADH)


