24B04: Exam Report
Compare and contrast the anatomy and physiology of smooth and skeletal muscle.
53% of candidates passed this question.
The anatomy component of this question required a detailed description of both the macro and microstructure of skeletal and smooth muscle, noting the differences and similarities between them.
For skeletal muscle specific detail on the fibre arrangement, subtypes (I/IIA/IIB) and their innervation as well as the structure of the sarcomere, thick and thin bands and associated proteins was required.
It was then expected that candidates would provide a description of how these components are similar or different in smooth muscle including details of unitary and multi-unit smooth muscle arrangements.
When comparing the physiology of skeletal and smooth muscle, better candidates discussed not only the process of AP generation, propagation and stimulus, but also detailed sources of ATP, and highlighted the differences in requirements for energy of each muscle type.
Higher scoring candidates discussed specific membrane potentials, noting the unstable membrane potential of smooth muscle which does not exhibit a resting membrane potential.
15B11: Exam Report
Compare and contrast the anatomy and physiology of skeletal and smooth muscle.
23% of candidates passed this question.
It was expected answers would describe in detail the role of troponin, tropomyosin and calmodulin in mediating muscle contraction. Detail on the structure (histology) of the skeletal and smooth muscle cells was often lacking. Many answers omitted the mechanism of muscle relaxation.
L1i / 24B04 / 15B11: Compare and contrast the anatomy and physiology of skeletal muscle and smooth muscle
Definition
Skeletal Muscle
Striated muscle tissue which is under voluntary control of the somatic nervous system
Smooth Muscle
Involuntary non-striated muscle
Location
Skeletal Muscle
muscle
Smooth Muscle
Walls of vessels, organs: resp tract, skin, walls of hollow organs; uterus, stomach, intestines, bladder
Macroscopic
Skeletal Muscle
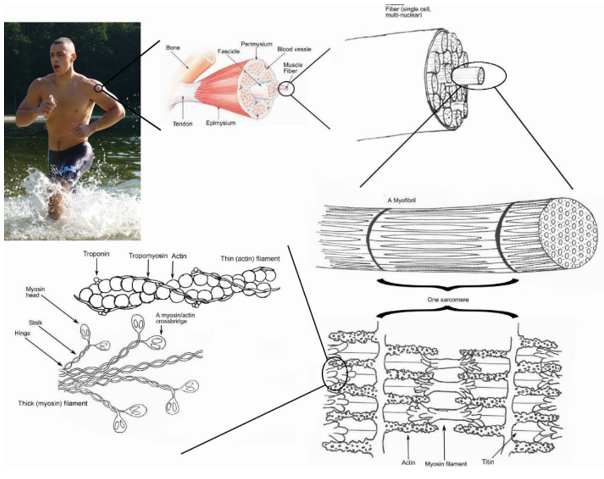
Motor unit = nerve ending + muscle fibres
Each fibre 10-100mm diam
Striated, ordered sarcomeres
Smooth Muscle
No striations = looks smooth
30-200mm LENGTH →thousands of times shorter than Sk m!
Microsopic
Skeletal Muscle
Multiple parallel myofibrils
Multi-nucleated
Mitochondria (aerobic & anaerobic metabolism)
SR (Ca++ storage)
Glycogen (E storage)
Myoglobin (O2 storage)
Smooth Muscle
One nucleus per cell
No striations → myosin and actin is disordered
No troponin
Calmodulin
Molecular
Skeletal Muscle
Sarcomere = functional unit
Contractile proteins = actin & myosin
- Myosin = heavy protein, long tail w 2 heads
- Actin = thin protein in double strands
Regulatory proteins = Tropomysin & Troponin
- Troponin: protein w 3 subunits
I – inhibits myosin ATPase
C- binds Ca++
T- binds Tropomysin
- Tropomysin – blocks actin/myosin interaction
Smooth Muscle
No RMP
Wandering membrane potential & resting tone
Autorhythmicity
Requires extracellular Ca++
For excitation-contraction-coupling
SR is poorly developed
Contractile proteins = Actin & Myosin
Regulatory Protein = Calmodulin
Innervations
Skeletal Muscle
Aa motor fibres
Smooth Muscle
Autonomic FIbres
Excitation-Contraction-Coupling
Skeletal Muscle
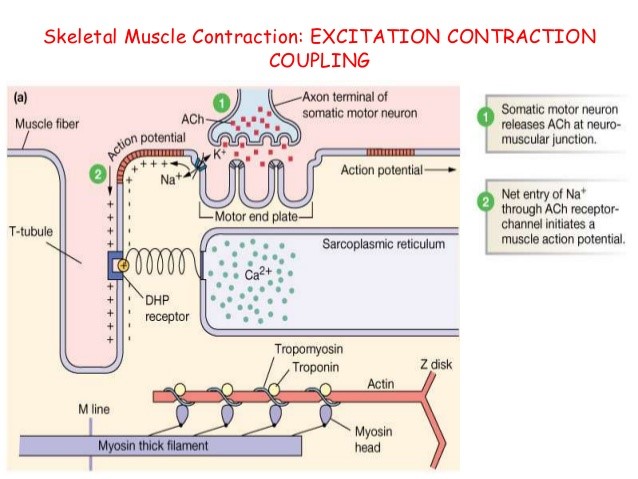
Sequence of events from AP → muscle contraction
Depolarisation of muscle end plate via nAchR
Threshold (-50mV) reached
AP propagates
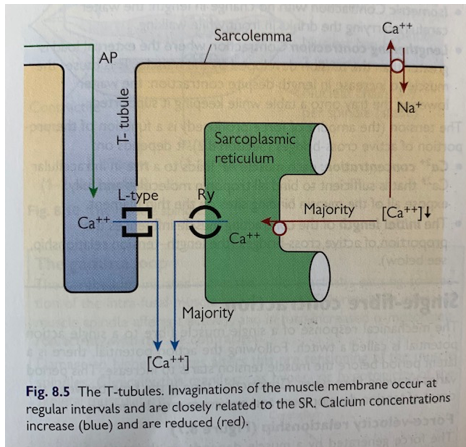
AP propagates along sarcolemma & down T-tubules
Activates L-type Ca++ ch of
T-tubles (see pic)
Flux of Ca++ intracellularly↑↑↑
Ryanodine Rec of SR open = mass x60↑ Ca++
Ca++ binds TnC
Removes inhibition of Troponin-Tropomyosin Complex
Exposes Actin binding site to myosin → commencement of cross-bridging
Myosin head pulls actin via ATP hydrolysis (ATPase) = contraction
Continues until Ca++ ↓
SERCA pumps Ca++ back into SR → relaxation
Smooth Muscle
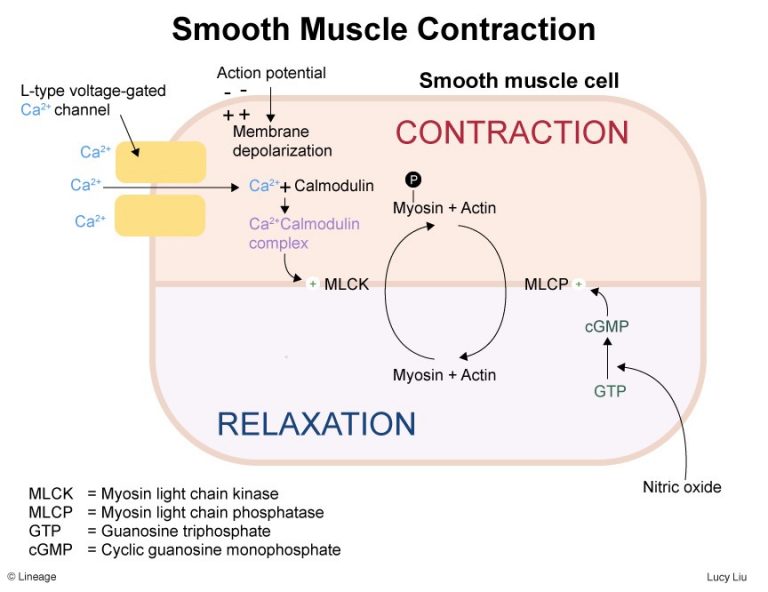
Wandering baseline membrane potential
(-40 to -60mV)
Depolarisation can be
- Spontaneous
- Ach binds muscuarinic rec (Gq) →IP3 →SR release Ca++
- Stretch
- Hormonal control
Threshold reached (-35mV)
Myocyte action propogates throughout smooth m via GAP JNS→ contraction
AP opens voltage gates Ca++ ch
Ca++ enters from ECF
Opens further Ca++ from SR (insignificant)
Ca++ binds calmodulin (cytoplasm protein
Ca-Calmodulin complex activates the enzyme myosin light chain kinase (MLCK)
Initiates myosin-actin cross bridge formation → contraction by conversion of ATP to ADP
Entire muscle fibre contracts together in a corkscrew manner
Muscle Contraction continues until ATP-dependent processes actively pump Ca++ out of the cell/into SR
Sm fns for long periods, without rest, but without using a lot of energy so some sm m can retain contraction despite Ca++ removal & MLCP by cross-bridging btw actin and myosin KA LATCH BRIDGING
MLCP → dephosphorelates myosin-ATPase
- Uncouples actin-myosin cross bridge
- ↓intrac Ca++
- Relaxation
Blood Flow
Skeletal Muscle
20% CO at rest
tightly regulated according to demands
Smooth Muscle
Skeletal Muscle Blood Flow
20% of CO at rest → 80% extreme exertion
1-4ml/100g/min resting → 100ml/100g/min
so there is a huge change in blood flow depending on demand:
- AUTOREGULATION
- Ability to maintain blood flow despite alterations in perfusion pressure
- Myogenic mechanism
- ↑pressure → VC → ↑resistance → ↓flow
- (&vice versa)
- METABOLIC
- High metabolic requirements
- Accumulation of many VD metabolites: CO2, H+, lactate, K, Adenosine
- ENDOTHELIAL
- Prostacyclin & NO synthesized by endothelium → VD →↑ flow
- MUSCLE PUMP
- Propulsion of blood with muscle contraction
- NEURAL
- Symp – major regulator of vessel tone during exercise
- a1 = VC
- b2 = VD
- HUMORAL
- Vasoactive hormones
- AII, ADR, NA, VASOPRESSIN, ANP, ENDOTHELIN, HISTAMINE, 5HT3