19A17: Exam Report
Explain the physiology of neuromuscular transmission.
60% of candidates passed this question.
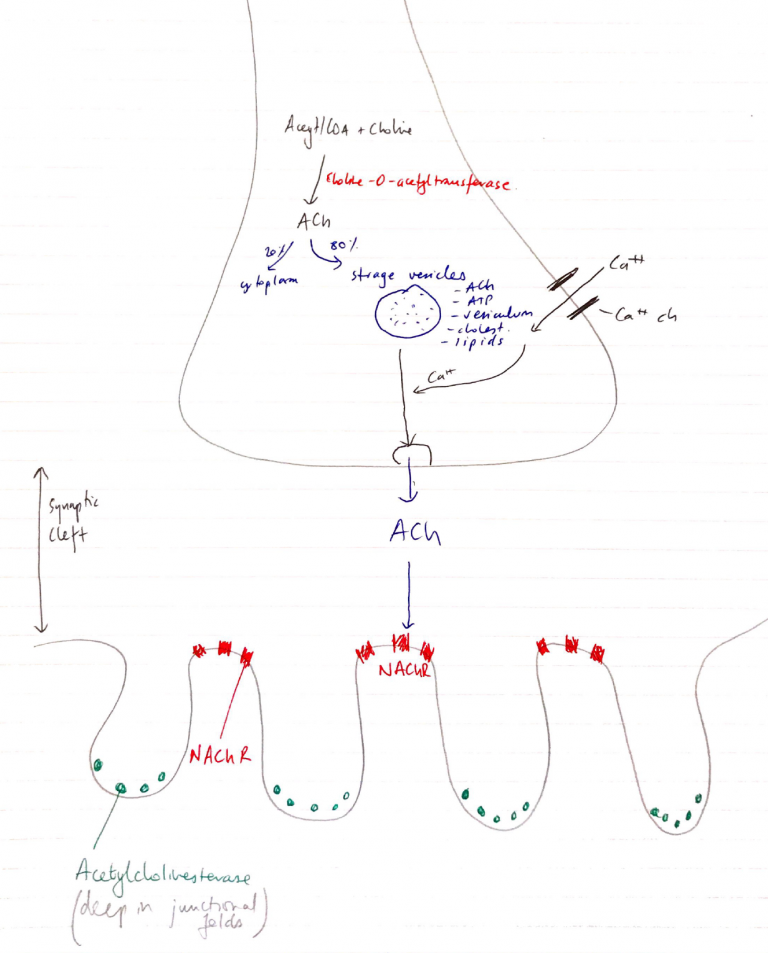
Description of sequential events from axon conduction to detail at the neuromuscular junction was required. Well-constructed answers defined neuromuscular transmission, elucidated the structure of the neuromuscular junction (best done with a detailed diagram), described the central importance of acetylcholine, including synthesis, storage, receptors, and degradation. An ideal answer also described both pre-synaptic (e.g. voltage-gated calcium channels, exocytosis of vesicles) and post-synaptic events (acetylcholine receptors, end plate potentials, and the events that lead to excitation-contraction coupling in skeletal muscle).
L1ii / 19A17: Explain the physiology of neuromuscular transmission
Definition
- NMJ = interface between nervous system & skeletal m.
- NT = ACh
- Skeletal m. innervated by Aα motor neuron
- Aa = large diameter, myelinated, arise from anterior horn SC
- At muscle, Aα axon divides into branches
- Each axon forms a single junction with a muscle fibre
- 1 group muscle fibres innervated by 1 motor n. = MOTOR UNIT
- Each Aα motor n. can innervate 1 – 2000 muscle fibres
- But each muscle fibre only supplied by 1 Aα motor n.
Anatomy
- Aα motor n. approaches muscle → loses myelin & branches into ‘Terminal Buttons’
- Muscle membrane opp Terminal Button is invaginated to form JUNCTIONAL FOLDS
- NAChR is at the top of fold → Anti-cholinesterase enzymes located in valley of folds
- Space b/w Motor End Plate & Terminal Button KA JUNCTIONAL CLEFT
ACh Synthesis & Release
- Nerve cytoplasm: Acetyl CoA + choline → ACh
- 80% stored in vesicles, 20% stored in cytoplasm
- ACh vesicles transported to NMJ
- AP arrives at Terminal Button
- Ca2+ influx at presynaptic terminal
- Vesicle fuses with membrane
- Releases contents into NMJ
- Delayed opening K+ channel then restores membrane potential
NAChR & Events Leading To E-C-C
- 5 units: 2 α, β, γ
- One ACh binds 2 x subunits (+ve cooperativity)
- Channel opens = ↑ permeability to cations (Na, K, Mg)
- Na+ INFLUX (biggest flux), K+ OUTFLOW (down their [ ] gradient)
- Allow depol. of sarcolemma which allows an End Plate Potential (EPP) of -55mV to be reached
- Reaching EPP allows AP to propagate along entire sarcolemma (i.e. muscle AP)
- The AP propagated along sarcolemma → down T tubules
→ Activates DIHYDROPYRIDINE RECEPTORS (voltage gated Ca2+ channels)
→ Ca2+ released → further ↑Ca2+ from adjacent RYANODINE RECEPTORS → mass ↑↑↑Ca2+ intracellularly
Motor Nerve Action Potential
- Motor n. RMP -90mV
- 2 types depolarisation because 2 types ACh release:
1. Spontaneous ACh Release
- Vesicles in Terminal Button randomly fuse with presynaptic membrane
- Release ACh into Synaptic Celft
- Small electrical 1mV charge
- KA Miniature End Plate Potential (MEPP)
2. Mass ACh Release
- Arrival of AP to Terminal Button
- Ca2+ influx presynaptic terminal
- 200 vesicles, containing 1500 ACh each, released into Synaptic Cleft
- Depolarises post-synaptic membrane 50 – 75mV
- Results in End Plate Potential (EPP)
NB: Each nerve releases x 10 amount of ACh needed → margin of safety for normal neuromuscular transmission