17A01: Exam Report
Outline the anatomy and physiology of the parasympathetic nervous system.
32% of candidates passed this question.
An efficient way to answer this question was to describe the anatomy and physiology of both cranial and sacral sections together. High scoring answers included an outline of the relevant nerves, the various ganglia, neurotransmitters and physiological effects. Some candidates described the cellular basis of Nicotinic, Muscarinic and M1-M5 receptors which didn’t attract marks.
14B04: Exam Report
Outline the anatomy and physiology of the parasympathetic nervous system.
0% of candidates passed this question.
Generally there was a lack of detailed knowledge, incorrect facts and at times confusion between the sympathetic and parasympathetic nervous system functions. A lack of anatomical detail was common (the origin of preganglionic cell bodies was not described clearly, and parasympathetic ganglia were not often named and located). It was expected an answer would mention the central role of Acetylcholine as a neurotransmitter at preganglionic and post ganglionic neurons in the parasympathetic system. Target organs were identified correctly but the exact action was not specified e.g. pupillary constriction vs. dilatation, GI sphincter/bladder – contraction vs. relaxation. Detail concerning receptor physiology was not required.
This is a question covering a core topic that no candidate passed. An overview of the arrangement and function of the autonomic nervous system is provided in several core physiology texts, including Ganong and Guyton.
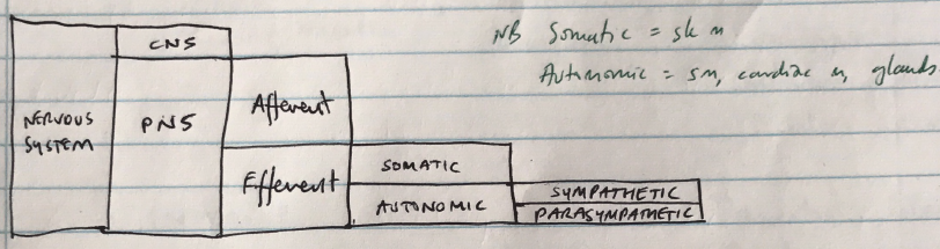
M1i / 17A01 / 14B04: Anatomy & physiology of the parasympathetic nervous system
Parasympathetic Anatomy
Preganglionic Neurons
- Myelinated B fibres
- Long preganglionic fibres
- Passes uninterrupted to ganglia near target organ
- Craniosacral outflow
- Preganglionic NT = ACh → acts on nicotinic receptors at ganglia
Postganglionic
- Unmyelinated C fibres
- Short due to location of ganglion near target organ
- Postganglionic NT = ACh → acts on muscarinic receptors
Cranial Nerves
Preganglionic fibre origin
Ganglion
Postganglion Fibre Target
III
→ from oculomotor nucleus
→ ciliary ganglion
→ Eye
- Ciliary m.
- Iris sphincter
- Pupil constriction
VII
→ Superior salivary nucleus
→ submaxillary ganglion
→ Submaxillary & sublingual
- Salivary glands
- ↑saliva secretion
IX
→ Inferior salivary nucleus
→ otic ganglion
→ Parotid gland
- ↑saliva secretion
X
Vagus is the major component of parasympathetic outflow
→ Accounts for 75% of parasympathetic fibres
→ Dorsal nucleus of vagus (X) in medulla
→ Ganglia of visceral plexuses
→ Cardiac plexus, SA node, AV node, conducting system
- ↓chronotopy, chronotropy, conductivity
→ Pulmonary plexus
- Bronchoconstriction
→ Gastric plexus
- Stomach, liver, spleen
- ↑GI motility & secretions
- Sphincter relaxation
- ↑peristalsis
Sacral nerves
S2, 3, 4 of spinal cord
→ Hypogastric plexus
→ Descending colon, rectum, bladder, uterus
- Rectal contraction
- Anus relaxation
- Uterine relaxation
- Contraction of detrusor m. in bladder wall
CHARACTERISTIC
PARASYMPATHETIC
Origin
Fibre length
Long preganglionic, short postganglionic
Preganglionic fibre
Myelinated B fibre
Ganglia location
Close to effector cells
Preganglionic NT
ACh
Ganglia receptors
Nicotinic
Postganglionic fibres
Unmyelinated C fibres
Postganglionic NT
ACh
Postganglionic receptor
Muscarinic
Function
Conserves & stores E.
ORGAN
ACTION
RECEPTOR
Heart
– inotropy
– chronotropy
– chronotropy
M2
Arteries
Dilatation
NB: not much effort on art/vein as for sympathetic NS
Lung
Bronchial constriction
↑bronchial gland secretion
M3
GI
↑motility
Sphincter relaxation
M3
M3
Liver
Glycogen synthesis
β2 + α
Kidney
Renin release
β1
Bladder
Detrusor contraction (voiding)
M3
Eye
Pupil constriction
↑lacrimal gland secretion
M3
M3
Submandibular & parotid glands
↑salivary secretion
M3