23B10: Exam Report
Outline the impact of sedative agents on thermoregulation (40% marks). Describe the physiological effects of a low body temperature (60% marks)
66% of candidates passed this question.
The first part of the question required candidates to outline the impact of sedatives on the interthreshold range with an explanation of what this is, how heat is lost, how heat generation is impaired and the mechanism by which these occur (ie. radiation/conduction/convection via vasodilation, with absence of vasoconstriction/heat generation strategies).
The second part of the question required a systems based approach with an outline of the perturbation as a result of the low body temperature. Temperature thresholds for certain physiological effects ie. loss of consciousness or arrhythmia was also expected for an overall thorough answer to this question.
22A16: Exam Report
Outline the impact of sedative agents on thermoregulation (40% marks) and describe the physiological effects of a low body temperature (60% marks)
33% of candidates passed this question.
Sedation reduces body temperature by interfering with heat production and increasing heat loss, along with widening of hypothalamic inter-threshold range.
This portion of the question was generally well answered. The question asked to “outline” the answer. Many candidates actually “described” the thermoregulation process in general but were unable to relate those with the impact of sedation.
The second part of the question (physiological effect of low body temperature) was answered by most of the candidates with the structure of organ-system wise description.
A few candidates scored extra marks by relating these effects with degree of hypothermia and by describing how thermogenesis responses (including shivering) can influence those effects. Some candidates restricted their answers to the effect of thermogenesis in response hypothermia and did not include the overall physiological consequences of low body temperature.
Better answers displayed an understanding of core temperature regulation, inter-threshold range and the effects of sedatives on thresholds for thermogenic responses, although only a few mentioned gain and maximal response. Better answers included specific detail (mentioned bradyarrhythmia, slow AF, VF, prolonged PR/QRS / J waves rather than just stating arrhythmia) across several organ systems.
Marks were not awarded for generic statements such as ‘decreased liver function’ without some additional detail. Inadequate depth of knowledge was main reason behind overall poor scores.
R1iv / 23B10 / 22A16: Outline the impact of sedative agents on thermoregulation (40% marks) and describe the physiological effects of a low body temperature (60% marks)
Impact of sedative on thermoregulation
1. Resetting of inter-threshold range
- Interthreshold range: Defined as a range of core body temperatures over which NO autonomic thermoregulatory responses are triggered → normally 0.2-0.4°C (36.6 – 37.0°C)
- ↑ width of range from 0.4°C to 4°C → ↓ threshold to cold by 3°C and ↑threshold to heat by 1°C → ↓thermoregulatory responses to Δ in body temperature
- Caused by a central effect → GA agent interferes with normal hypothalamic function to maintain a narrow threshold range
2. Vasodilation
- Sedative-induced vasodilation secondary to sympathectomy (blunted efferent outputs) → redistribution of heat from central to peripheral compartments
3. ↓ BMR
- Sedative-induced ↓ BMR / heat production by 20-30%
4. Altered Behavioural Response
- Due to altered conscious state & paralysis; unable to seek shelter, clothes etc
5. Loss of Shivering
- Dexmedetomidine and clonidine markedly reduce shivering threshold
6. Increase Sweating Threshold
- Propofol, dexmedetomidine, clonidine
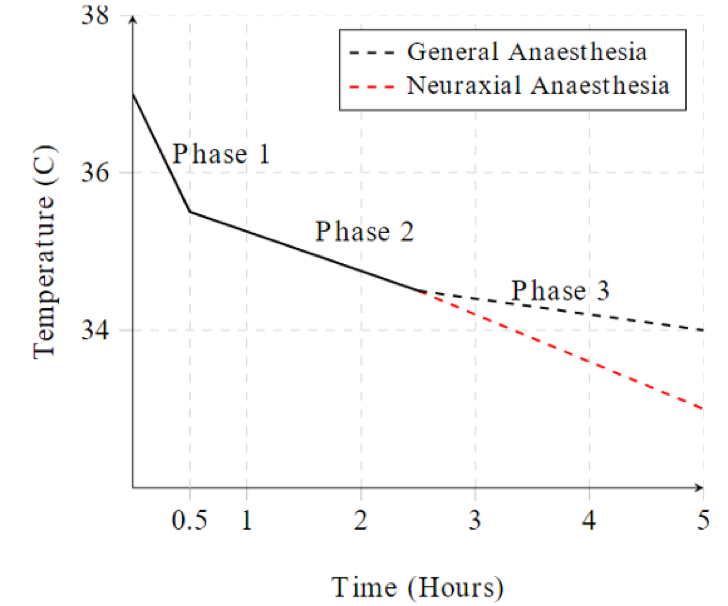
Phase 1
Redistribution of heat from core to periphery due to peripheral vasodilation à loses 1C core temp in first hour
Phase 2
Gradual Linear Decline over 2-4h as heat loss > metabolic heat production
Phase 3
Plateau in core temperature when heat loss = metabolic heat production
Physiological effects of low body temperature
Definitions
- Normothermia: 37°C +/- 0.4°C
- Hypothermia defined as core body temperature < 36°C
CVS
- ↑ HR initially then progressive bradycardia with ↑ cold
- ↑ Cardiac arrhythmias & myocardial ischemia due to catecholamines released from stress response (spontaneous VF <28°C)
- J waves on ECG → represents ↑ in phase 1 repolarization; prolonged PR interval, 1st degree heart block
- Resistance to defibrillation
- ↑ SVR & MAP due to peripheral vasoconstriction → ↑ afterload
- ↓ CO due to direct negative inotropic effect of cold & ↑ afterload / SVR
RESP
- Left shift in HbO2 dissociation curve: ↑ O2 affinity, ↓ O2 offloading to tissues
- V/Q mismatch secondary to inhibition of hypoxic pulmonary vasoconstriction
- Bronchospasms
- ↓ MV (and in severe cases apnea)
CNS
- Altered mental state (esp ↑drowsiness, unconsciousness, delayed awakening from GA)
- ↓ CBF
- ↓ CMRO2 by 6% for every 1°C ↓ in temperature
- ↓ in glutamate & oxygen free radical release
- Inhibition of inflammatory products (cytokines, interleukins, etc)
HAEM
- Coagulopathy (due to platelet dysfunction & loss of clotting factor enzyme function) → ↑ transfusion requirements due to bleeding
- Impaired coagulation cascade
- ↑ blood viscosity (haemoconcentration)
- ↓ WBC activity → ↑incidence of infections
Acid-Base
- Rise of pH with falling body temperature
- Fall of pCO2 with falling body temperature
RENAL
- Impaired renal function (oliguria)
- Cold diuresis → peripheral vasoconstriction resulting in central hypervolemia → ↓ ADH secretion → diuresis
GI
- Impaired hepatic metabolic function (esp ↓ drug metabolism, such as muscle relaxants action is prolonged)
- ↓ GI motility → ileus
Metabolic & Endocrine
- Impaired wound healing (due to catabolic state & wound vasoconstriction)
- ↑ protein catabolic state
- ↑ stress response (steroids & catecholamine released)
- Shivering (5x ↑general MRO2) → causes hypoxaemia (risk of myocardial & cerebral ischemia)
- In absence of shivering → general ↓ MRO2 (by up to 50%) and ↓ BMR
- BMR ↓ 6% for every 1°C drop in core temperature
- Hyperglycaemia due to ↓ cellular uptake of glucose
- Lactic acidosis can develop due to shivering and decreased tissue perfusion
Author: Novia Tan