R1iv: Additional – The effects of GA and Neuraxial Anaesthesia on Thermoregulation
Definition: Thermoregulation = the tight control of core body temperature despite fluctuating ambient temperatures
GA
- Causes core hypothermia
- Widens interthreshold range
- Reduces Cold Threshold 2.5C
- Increases Warm Threshold 1.3C
- Core temp at which thermoregulatory threshold triggers VC is agent & dose dependant
- Reduced Cold Response
- Heat loss 2 late VC
- Reduced heat production
- GA reduces BMR 30%
- Non shivering thermogenesis abolished
- Reduced threshold for shivering
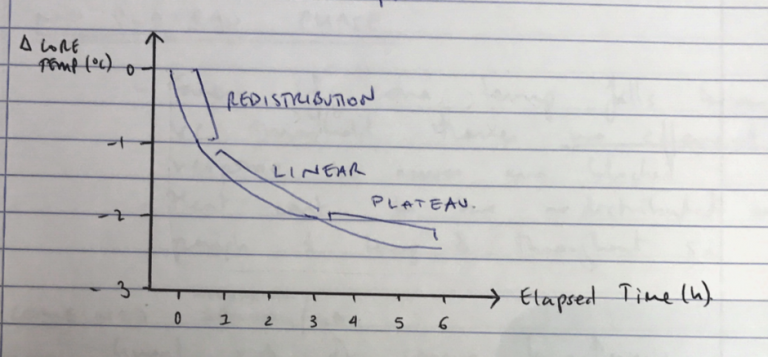
- Hypothermia ensues in 3 stages
Phase I: Internal Redistribution of Body Heat
- Rapid 1-2 degree fall in first hour of sedation
- VD by TIVA/volatiles → heat redistributed from core → mass heat loss by Radiation
- GA → widens interthreshold range and delays activation of compensatory VC → heat redistributed from core to peripheries
Phase II: Heat Loss > Heat Production
- Linear decline by 1 degrees over 2-3hrs by
- Radiation: Loss of VC = increased heat loss by radiation
- Conduction: heat loss by direct contact of patient w bed, probes, soiling
- Convection: Loss of errrector pili increases heat loss by convection, no wind currents in ICU therefore heat conservation by hospital gowns, but frequent exposure for examination, procedures & nursing checks
- Evaporation: insensible heat losses from skin & lungs, but loss of sweating mechanism
- Behaviour: inability to shiver and increase BME, seek warmth, clothing etc
- Equipment: indwelling catheters, ECMO, CRRT all increase heat loss by conduction, convection and radiation
- Overall Heat loss >> heat production
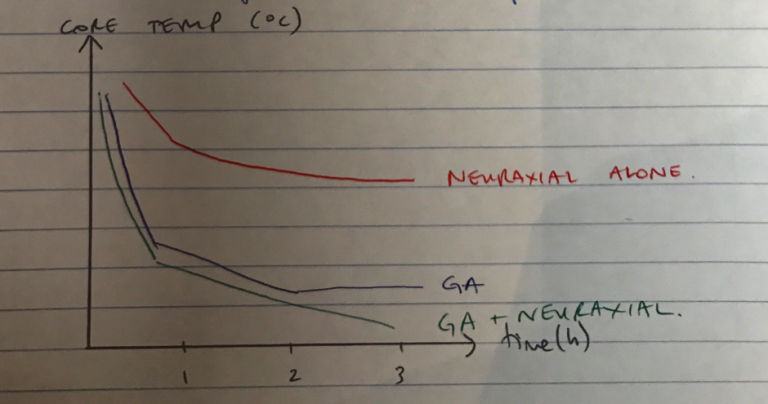
Neuroaxial
Definition: Injection of LA around nerves to blunt responses to pain, allowing patient to remain conscious
- Neural blockade blocks efferent limb of thermoregulatory response in lower half of body → VC, shivering, sweating
- Hypothermia develops → 2 phases, less marked
Phase I: Internal Redistribution
- Loss of VC
- Heat moves from core → peripheries
- 1C drop in 30mins
Phase II: Heat Loss > Heat Production
- Increase in peripheral temp = increased gradient for heat loss
- Combined w other factors contributing to heat loss during surgery
- Not as marked cf GA as BMR drop is less
- Rate of linear decline not as steep
No Plateau Phase
- Even if core temp falls below VC threshold, there is no efferent response as nerves are blocked
- Heat continues to be redistributed to peripheries and temperature drops throughout surgery