19A09: Exam Report
Classify antibiotics with respect to their mechanism of action (50% of marks). Outline the mechanisms of antimicrobial resistance (50% of marks). Give specific examples of each.
70% of candidates passed this question.
This question was well answered. Marks were awarded for correct pairing of mechanism of action and resistance with examples of drug class. Few mentioned the mechanisms by which resistance is present; acquired or generated.
T1ii / 19A09: This question was well answered. Marks were awarded for correct pairing of mechanism of action and resistance with examples of drug class. Few mentioned the mechanisms by which resistance is present; acquired or generated.
Definitions
Bacteria = Prokaryote – single cell organism lacking a nucleus or any membrane-bound organelles
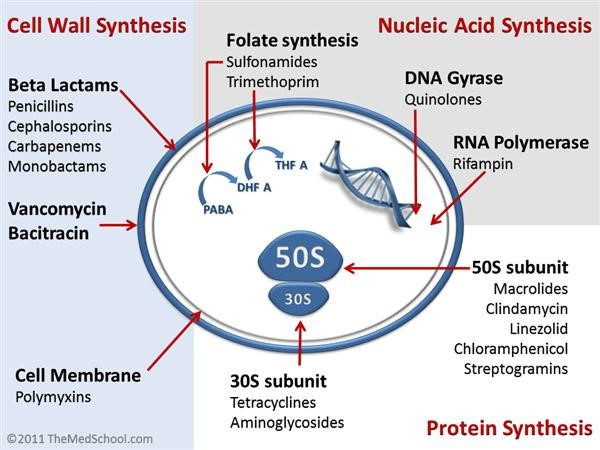
Cell Wall Synthesis Inhibitors
Penicillins
Cephalosporins
Vancomycin
Beta-lactamase inhibitors
Carbapenems
DNA Synthesis Inhibitors
30s Inhibition
Aminoglycosides
Tetracyclines
50s Inhibition
Macrolides
Chloramphenicol
Clindamycin
Linezolid
Protein Synthesis Inhibitors
Fluoroquinolones
Metronidazole
RNA Synthesis Inhibitors
Rifampicin
Mycolic Acid Synthesis Inhibitors
Isoniazid
Folic Acid Synthesis Inhibitors
Trimethoprim
Sulfonamides
Resistance = when the maximal level of the agent tolerated is insufficient to inhibit growth
- Natural – bacteria do not possess molecular target for that drug
- Acquired:
1. Modification of Antimicrobial Molecule
a. Chemical Alteration of the Antibiotic
- Production of enzymes capable of introducing chemical changes to the antimicrobial molecule
- Example: Aminoglycoside Modifying Enzymes (AMEs) which modify the hydroxyl/amino groups of the aminoglycoside, enabling resistance E Faecium
b. Destruction of the Antibiotic Molecule
- b-lactamases produced by bacteria hydrolyse the b-lactam ring
- ∴negates penicillin
- still sensitive to cephalosporins
- ESBLs = even more widespread resistance
- R to cephalosporins/penicillin/b-lactamase inhibitors (Clav Acid)
- Only Mero is effective
2. Prevention of Antibiotic Reaching Target
a. Decreased permeability
- Many a/b have targets inside bacteria or on their membrane
- Example: Vancomycin is not active against Gm- bacteria as it cannot penetrate the outer membrane
- Example: P aeruginosa is very good at altering porin fn/expression to limit permeability of a/b
b. Efflux pumps
- P aeruginosa possess an efflux system to pump a/b out of the cell
3. Change/Bypass of Target Site
- Changing of target site = ↓affinity of drug
- Example: VRE
- Glycopeptides bind to D-Ala-D-Ala
- Bacterial remodelling of cell wall to provide new substrate D-Ala-D-Lactate prevents Vancomycin binding
- Especially common in enterococci (E Faecium)
4. Resistance Due to Global Cell Adaptive Processes
- Example: Daptomycin resistance
- Altered cell wall metabolism resulting in changes in surface charge of the bacteria and produces an electrostatic ‘repulsion’ of Daptomycin from the cell wall of enterococci