21B06: Exam Report
Describe the functions of the placenta (80% marks). Outline the determinants of placental blood flow (20% marks)
49% of candidates passed this question.
There was a wide range of marks for this question with a few candidates scoring excellent marks. Those answers that scored well provided a comprehensive list of functions as well as an explanation as to the what, how and/or why of these functions. Poorer answers omitted some of the functions or failed to elaborate on them by providing only a limited list. The second component of the question was generally well outlined, most candidates provided some estimate of normal values at term and a simple elaboration regarding the factors that affect placental blood flow.
18A09: Exam Report
Describe the functions of the placenta (80% of marks). Outline the determinants of placental blood flow (20% of marks).
32% of candidates passed this question.
Many candidates provided a broad overview of functions of the placenta but lacked detail. Placental blood flow has maternal and foetal components, though most only considered the maternal circulation to the placenta and didn’t mention the foetal vessels. Many were not specific as to what blood vessels were described.
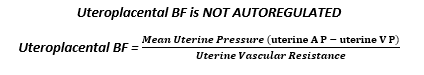
Many stated that uterine blood flow is not autoregulated, however went on to describe myogenic and neuro-humoral mechanisms of autoregulation.
V1ii / 21B06 / 18A09: Describe the functions of placenta (80 marks). Outline determinants of placental blood flow (20 marks).
DEFINITION – Placenta is an organ which provides an interface between mother & foetus
Quantify
- Disc shaped
- Wt 500g
- Length 20cm
- SA 15m2
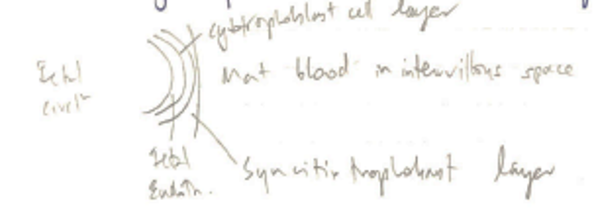
Structural Unit
- CHORIONIC VILLUS
- Villi = vascular projections from foetus
- Chorion = 2 layers
- Syncitiotrophoblast → direct contact with maternal blood in intervillous space
- Cytotrophoblast → Inner layer
- As villi mature → loose cytotrophoblast layer → single layer of syncitiotrophoblast & foetal capillary endothelium separating maternal & foetal blood
Blood Supply To Placenta
- Maternal circulation: mother, intervillous space
- Foetal circulation: foetus, umbilical cord, placental villi
- NB: maternal & foetal blood ≠ mix
Maternal blood:
- Uterine/ovarian arteries (oxygenated) → Arcuate → radial → spiral (which enter intervillous space)
- Pressures: 100mmHg (uterine a.) → 70mmHg (spiral a.) → 10mmHg (intervillous space)
Foetal blood:
- Foetal iliac arts → 2 umbilical a. → chorionic a. (deoxygenated) → capillaries enter villi
- Maternal BF x 2 ≥ umbilical BF
- ∴Improving efficiency for substance transfer
- Substances from maternal blood → through synciotiotrophoblast → foetal caps → chorionic veins → 1 umbilical vein
Control of Uteroplacental Blood Flow
- Normal Uterine BF (non-pregnant) = 100mL/min
- @ term, uteroplacental BF = 600mL/min (10% of maternal CO)
→ 90% placenta
→10% non-placental tissue
- To accommodate ↑BF → T. Media (elastic + muscular) layer of vessels is replaced with fibroid cells to allow maximal dilatation
- Uterine arteries still maintain α-adrenal receptors
↓ Uterine BF with ↓ Uterine A P
↓ Uterine V P
↑ Uterine Vasc. Resistance
Aorto-caval compression
Hypovolaemia
Sympathetic block 2° non-axial anaesthesia
Vena cava compression
Uterine contractions
Valsalva
Catecholamines
Vasopressin release (2° hypovolaemia)
Compression of spiral a. during contraction
Exogenous vasopressors
Functions of the Placenta
- RESPIRATORY
- ENDOCRINE
- NUTRITION
- IMMUNOLOTY
Respiratory
- Foetal lungs do not partake in gas exchange
- Placenta transfer O2/CO2 to/from foetus
- Oxygen
- O2 transfers via DIFFUSION from partial pressure gradient
Bohr Effect
- Maternal blood takes up foetal CO2
- Becomes more acidotic
- Causing Hb to release O2 more readily (BOHR)
- Favours O2 release to foetus
Double Bohr Effect
- Foetal blood releases CO2 to maternal blood
- Foetal blood more alkalotic
- L) shift foetal ODC
- Favours foetal O2 uptake
HbF
- Shifts foetal ODC L)
- Further favours foetal O2 uptake
Carbon Dioxide
- Passive DIFFUSION down partial pressure gradient
Haldane Effect
- Maternal blood releases O2
- Maternal Hb becomes ‘deoxygenated’
- ∴can carry more Hb as HCO3– & carbamino compounds
Double Haldane Effect
- Foetal blood takes up O2
- Hb ↓ affinity for CO2 → released to maternal circulation
Endocrine
- Placenta produces steroid & peptide hormones:
- HCG
- stimulates C. Luteum to secrete P which maintains viability of pregnancy
- Human Placental Lactogen (HPL):
- ↓ maternal insulin sensitivity → ↑BGLs
- Foetal pulmonary surfactant production
- Mobilises FFAs → sparing glucose for foetus
(Converts mother from 1° glucose → 1° FA user)
- Promotes maternal breast milk development
- O & P
- O stimulates uterine growth & mammary gland development
- Placenta takes over from C. Luteum @ 8 weeks
- 1° P secretion
- P causes muscle relaxation & prevents labour onset
Nutrition
- Placenta transports nutrients to meet foetal requirements
PASSIVE
ACTIVE
PINOCYTOSIS
O2
CO2
H+
HCO3–
Urea
Na, K
Lactate
Gluclose
Amino-acids
FFAs
IgG
Immunological
- IgG Ab’s cross mother → foetus by PINOCYTOSIS
- Provides passive immunity first four months of life