23A15: Exam Report
Describe the adult coronary circulation (50% of Marks) and its regulation (50% of Marks)
66% of candidates passed this question.
For this question a good answer should have encompassed a description of the following components; the arterial supply (epicardial, endocardial supplies), venous supply (major and minor venous drainage), the phasic ventricular blood supply a description of and the relevance of the high oxygen extraction ratio, an emphasis on metabolic autoregulation whilst including any other mechanisms of physiological regulation.
Most candidates provided reasonable detail surrounding the arterial-circulation and the area of the heart these vessels supply. Less well described were the perforating branches, the capillary network and the venous drainage, these components were often incorrectly described or left out of the candidate answers.
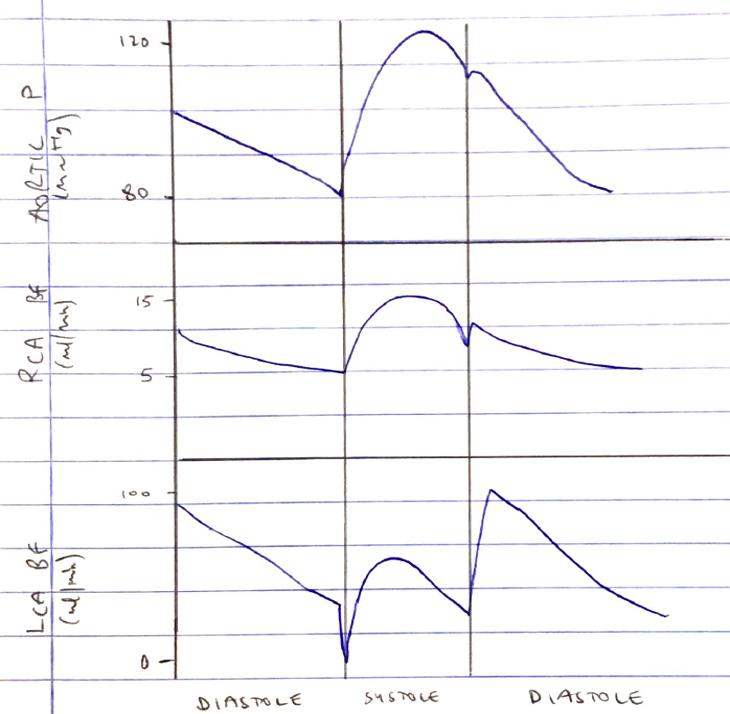
Most candidates correctly identified the phasic flow and the difference in flow that occurs between the right and left ventricle. Those candidates that used diagrams to explain this were rewarded when these diagrams were labelled and accurate with respect to their systolic and diastolic distinction.
The control of regulation was less well answered with generic statements not specifically identifying the local metabolic controls importance over any other mechanism. Those answers that scored well coupled the metabolic control to the flow dependence highlighting the high oxygen extraction within the coronary circulation.
21A19: Exam Report
Describe the adult coronary circulation (50% marks) and its regulation (50% marks)
62% of candidates passed this question.
Good candidates described normal blood flow to the coronary circulation, including differences between the right and left ventricles. Coronary artery anatomy was outlined, including the regions of the heart supplied and the concept of dominance. In addition to epicardial vessels, strong answers also outlined penetrating arteries, subendocardial supply and venous drainage. Regulation of coronary blood flow required an explanation of flow-dependence of the heart given its high oxygen extraction rate. Metabolic autoregulation and its mediators needed to be described, along with the physical factors driving coronary blood flow. Less important mechanisms such as the role of the autonomic nervous system were also described, with an emphasis on indirect effects over direct effects.
18A11: Exam Report
Describe the regulation of the coronary circulation.
46% of candidates passed this question.
Some answers suffered from listing things rather than describing things as the question required.
Better answers included a description of metabolic, physical and neuro-humoral factors and the relative importance of each.
Many described detailed anatomy which was not necessary.
14B10: Exam Report
Describe the adult coronary circulation (50% of marks) and its regulation (50% of marks).
65% of candidates passed this question.
This question was generally well answered. Some candidates did not mention the factors which are peculiar to the coronary circulation and answered in a generic manner, as if for any vascular bed. The coronary circulation has a high O2-ER and flow-dependence.
Many candidates seemed to lack a perspective that metabolic demand dominates control of the coronary arterial flow. The phasic nature of flow was best shown with a diagram and whilst “publication-level” graphs are not expected, the graph drawn must be factually correct and convey the principal similarities and differences. While this topic is covered in both Guyton and Ganong, additional detail can be found in the Mosby physiology monograph series: Cardiovascular Physiology, 10th Edition by Pappano and Wier,( the replacement of Berne and Levy).
G1ii / G4iii / 23A15 / 21A19 / 18A11 / 14B10: Describe the adult coronary circulation (50 marks) and its regulation (50 marks)
Anatomy
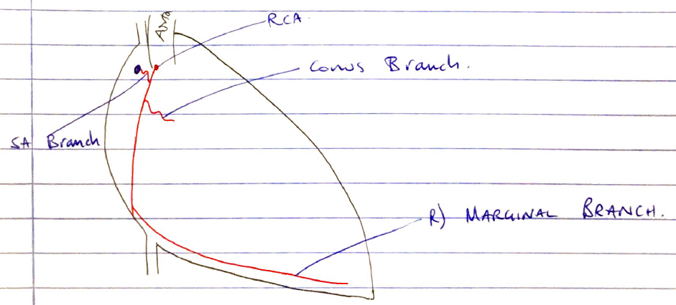
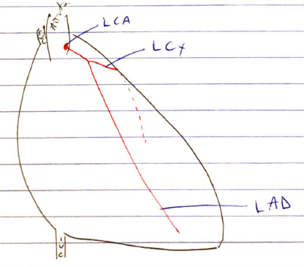
RCA: supplies RA & RV
- Comes off aortic root from R) coronary ostium from R) cusps of Aorta
- Gives off:
- Conus br.
- SA br. → SA Node
- R) marginal br. → inf. border
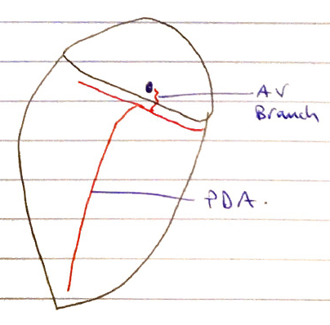
- Post Descending A. → inf. LV wall, 1/3 septum
- AV Nodal br.
60% population is RCA dominant = supplies POA & AV br.
- SA Node = in wall of RA lateral to entrance of SVC
- AV Node = in intra-atrial septum, next to opening of coronary sinus which opens into RA
Coronary Venous Circulation
- CORONARY SINUS = collection of veins that collect blood from myocardium
- Drains into RA between AV orifice & IVC orifice
- Tributaries: small, middle, great, oblique veins
- ANTERIOR CARDIAC VEINS → drain directly into RA
- THEBESIAN VEINS → do not drain into coronary sinus
= small valveless veins in walls of all heart chambers
- Most abundant in RA
- Thebesian vessels of LA & LV, together with bronchial veins, contribute deoxygenated blood to systemic circulation which makes up “physiological shunt”
RCA + LCA = EPICARDIA ARTERIES → low R distribution vessels
INTRAMUSCULAR ARTERIES → divide & penetrate myocardium (resistance vessels) & form the dense cap network of myocardium
Coronary Blood Flow
- Normal CBF = 250mL/min = 5% CO
RCA
- Significant CBF during systole & diastole
- Lower pressure generated by their RV in systole ∴more driving pressure
LCA
- Early systole → extravascular compression → CBF briefly reversed
- Mid-late systole → follows aortic P
- Early diastole → L) CBF is maximal when there is ventricle relaxation & no extravascular compression
- Then L) CBF falls as aortic P falls
- \( \textbf{CBF = } \frac{ \text{CEREBRAL PERFUSION PRESSURE} }{\text{CEREBRAL VASCULAR RESISTANCE}}\)
Coronary Perfusion Pressure
- Perfusion pressure is the driving pressure (gradient) for blood flow
- In most organs, perfusion pressure is the gradient between:
Arterial supply P – venous drainage P
- Heart CBF operates a Starling Resistor Mechanism
- ↑extravascular P from myocyte contraction = Starling Resistor
- Aortic/Diastolic P = driving P
- Ventricular P = Starling resistor
- RAP (coronary sinus P) = venous drainage P
- ∴CPP = Aortic Diastolic P – Ventricular P/RAP (larger of)
- Diastolic Aortic P used because:
- LV has larger muscle mass
- Most CBF goes to LV
- There is no CBF to LV in systole
- Most flow occurs in diastole
NOTE: there are different pressures in the Aorta & Ventricle/RAP, depending on the phase of the cardiac cycle
That is why there is phasic CBF
- LV Systole CPP = Aortic Systolic P – LV intraventricular P
= 120 – 120
= 0mmHg
- LV Diastole CPP = Aortic Diastolic P – RAP
= 80 – 5
= 75mmHg
(Here we take RAP which is larger than Ventricular P, which is 0mmHg in diastole)
- RV Systole CPP = Aortic Systolic P – RV intraventricular P
= 120 – 25
= 95mmHg
- RV Diastole CPP = Aortic Diastolic P – RAP
= 85 – 5
= 75mmHg
Coronary Vascular Resistance
- Resistance to flow through a vessel was described by Poiseuille
- \( \textbf{R = } \frac{\text{8hL}}{\text{πr4}} \)
- η= blood viscosity
- L = vessel length
- R = radius
- Radius has the largest influence (to the power 4) on resistance to flow e. ↓diam. 50% = ↑R x 16
- ∴Resistance in coronary vessels affect by:
- VISCOSITY
↑ viscosity = ↑R = ↓flow
- LENGTH
r length = ↑R = ↓flow
- RADIUS
↑radius = ↓R = ↑flow
- Radius of CA affected by:
- Pathology (vasospasm, atheroma)
- Metabolic
- Myogenic autoregulation
- ANS
- Humoral
- Drugs
- Radius of CA affected by:
Metabolic
↑metabolic demand = ↓O2 supply = production of BD metabolites
- Adenosine
- H
- K
- CO2
- Lactate
- NO
All above VD coronary vessels
Myogenic Autoregulation
CPP kept constant between 60 – 180mmHg. Smooth muscle cells contract & relax in response to ∆ transmural pressure
ANS
- α1 receptors → epicardial vessels → VD
- β2 receptors → subendocardial vessels → VC
- influence is weak. Baseline symp. VC tone
Humoral
- VD: adenosine most potent → ↓ATP = ↑ADP = ↑Adenosine
- Α1 receptor = ↓HR, ↓FOC
- A2 receptor on smooth m. = Coronary a. = VD
- VC: endothelium, AII, ADH (stress)
Drugs
- Nicorandil = K+ channel opener = hyperpolarisation = VD
- CCB + nitrates = VD
Myocardial O2 Supply + Demand
- CBF = 250mL/min = 5% CO
- Heart = has highest O2 consumption for any organ
- Arterial O2 extraction = 80% (25% for other tissues)
- Because O2 extraction is so high, any ↑O2 demand must be met with ↑flow = FLOW LIMITED
- pO2 of coronary sinus blood = 20mmHg
O2 supply to myocardium
- O2 content
- CaO2 = (1.34 x [Hb] x SpO2) + (PaO2 x 0.003)
- \( \text{CBF = } \frac{\text{CPP}}{\text{CVR}} \)
- HR
- ↑HR = ↓time in diastole = ↓CBF
Myocardial O2 consumption
- At rest = 8mL/100g/min (20 x greater than skeletal m.)
- @ Exercise ↑300 – 400mL/100mg/min
- Myocardial Wall Tension = 40% consumption → preL, afterL, contractility
- Heart rate = 15%
- Basal metabolism = 25%
- Electrical activation = 1%
- External work = (rest)