G3iii: Regulation of the heart
CO = HR x SV
- Determinants of myocardial performance
- HR
- PreL
- AfterL
- Contractility
- Regulation of Cardiac Performance
- INTRINSIC
- Pacemaker activity
- Frank-Starling Mechanism
- EXTRINSIC
- Neural
- Hormonal
- Chemical/Metabolic
- Drugs (do not regulate, but influence)
- INTRINSIC
Intrinsic Regulation
- Intrinsic Pacemaker Activity
- The heart can initiate its own beat in absence of neural/hormonal control
- Intrinsic rate of discharge of SA Node ~100bpm (in absence of autonomic influences. This is KA INTRINSIC HR)
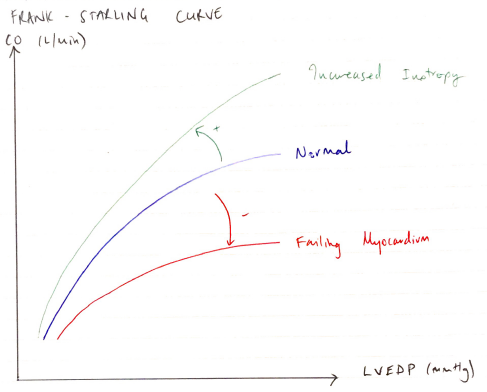
The Frank-Starling Mechanism
Frank-Starling Law states the ability of the cardiac muscle fibre to contract is dependent upon, and proportional to, its initial fibre length
- An intrinsic cardiac adaption
- Extra blood flows into ventricles
- Results in ↑preload
- Increases sarcomere length
- ↑FoC generated because there is ↑actin/myosin overlap
- This continues to occur with ↑preload until an optimum preL is reached → optimal resting sarcomere length = 2.2µm
- Excess high filling pressure → myocardial fibres over stretch → ↓FoC
- This important intrinsic adaption allows CO to match VR of the R & L ventricles
- This is displayed by the FRANK-STARLING CURVE
- ↑preL causes patient to shift along curve, resulting in ↑CO with each contraction
- ↓preL will cause the opposite
- Whole curve can be shifted with + INOTROPY or CARDIAC FAILURE
- +ve inotropy → ↑CO for a given preL, shifting curve UP & LEFT
- Myocardial failure → for any preL, CO will ↓, shifting curve DOWN & RIGHT
Extrinsic Control
- ANS
- Cardiac reflexes
- Hormones
- Temperature
- Metabolic/Electrolytes
- Drugs (do not regulate, but influence)
Autonomic Innervation of the Heart
Efferent Nerve Fibre Origin
Parasympathetic
- Cell bodies in Medulla
- Collections KA DORSAL VAGAL NUCLEUS & NUCLEUS AMBIGUUS
Sympathetic
- Vasomotor Centre in ROSTRAL VENTROLATERAL MEDULLA
Efferent Nerve Pathway
Parasympathetic
- Exits at CN X (Vagus)
- As R+L vagal branches synapses in/near Epicardium & Myocardium + near SA & AV Node
Sympathetic
- PREGANGLIONIC: inferomediolateral grey columns of SC
- GANGLIA: paravertebral chain
- POSTGANGLIONIC: supracardial plexus & adventia layer of blood vessels
NT Receptors Intracellular Response outcome
Parasympathetic
- Ach
- Muscarinic
- M2 Receptors
- Gq→ ↑K+ → membrane hyperpolarisation
- ↓HR (↓automaticity)
- ↓transmission through AV Node
- ↓Contractility
- Slows relaxation in diastole
Sympathetic
- ACh & NA → β1 receptors
- GS → ↑cAMP → ↑Ca2+
- ↑Inotropy
- ↑Chronotropy
- ↑Automaticity
- Coronary VD
- ↑dP/dt
DoA
Parasympathetic
- Rapid onset & offset due to AChE
Sympathetic
- Slow onset but longer lasting due to amplification by 2nd messenger system
Basal Tone
BaroR Reflex
Parasympathetic
- Predominates at rest
- Stimulatory
Sympathetic
- ↓symp. activity at rest
- Inhibitory
Cardiac Reflexes
- Definition: a fast-acting loop between H & CNS
- Consists of:
- Afferent Sensor (monitors cardiac function) in atria, ventricles, CA, great vessels
→ Control (CNS)
→ Effector organ (ANS)
- Function: to maintain constant CO & critical organ perfusion
- The 6 Cardiac Reflexes
- BaroR
- ChemoR
- Bainbridge
- Bezold – Jarisch
- Cushing’s
- Oculocardiac
Reflex Sensor
Afferents
Baroreceptor Stretch
Baroreceptors in aortic arch
Carotid sinus
Chemoreceeptor Chemo
Carotid + aortic bodies
Bainbridge Stretch
RA wall
Cavoatrial junction
Bezold-Jarisch Chemo & Mechano
Ventricle wall
Unmyelinated Type C fibres
Cushing’s
CNS
Oculocarrdiac
Extra-ocular muscle & globe
Reflex Sensor
Stimulators
Baroreceptor Stretch
↑Transluminal pressure
Chemoreceeptor Chemo
pO2 <80
pO2 >40
pH <7.4
Bainbridge Stretch
Stretch
↑filling
Bezold-Jarisch Chemo & Mechano
Noxious stimuli
Cushing’s
Ischaemia 2° ↑ ICP
Oculocarrdiac
↑pressure
Reflex Sensor
Control
Baroreceptor Stretch
Via glossoph. (carotid)
Vagus (arch) to CV Centre of Medulla
Chemoreceeptor Chemo
Via glossoph. (carotid)
Vagus (aortic) to CV Centre of Medulla
Bainbridge Stretch
Via vagus (X) to CV Centre in CNS
Bezold-Jarisch Chemo & Mechano
Medulla vasomotor centre
Cushing’s
Direct symp. stimulation of vasomotor centre
Oculocarrdiac
Ciliary nerve to Trigeminal
Reflex Sensor
Efferent
Baroreceptor Stretch
NEGATIVE FEEDBACK inhibits symp. & ↑parasymp. nerves
Chemoreceeptor Chemo
- Stimulates resp centre
- ↑SNS
- ↑catecholamine release from Adrenal Medulla
Bainbridge Stretch
PNS inhibition = ↑HR
Directly stimulates SA node = ↑HR,↑ANS, ↓ADH
Bezold-Jarisch Chemo & Mechano
↑PNS activity
Cushing’s
MASS SYMP. STIMULATION
Oculocarrdiac
Vagus
↑PNS
Reflex Sensor
Overall effect
Baroreceptor Stretch
@Heart
- ↓HR
- ↓FoC
- ↓CO
@Vessels
- ↓VR
- ↓venous/ arterial tone
Chemoreceeptor Chemo
- ↑MV
- ↑HR
- ↑FoC
- VD CA
- ↑SVR
Bainbridge Stretch
- ↑HR
- ↑NaCl/H2O excretion
- ↑urine output
Bezold-Jarisch Chemo & Mechano
Triad of:
- ↓HR
- ↓BP
- ↓SVR
Cushing’s
- ↑HR
- ↑BP
- ↑FoC (to trigerminal & ↑CAP)
- BaroR
- Reflex brady
Oculocarrdiac
- ↓HR
- ↓Foc
- ↓BP
Hormones
Catecholamines
- Adrenaline & NA released by Adrenal Medulla
- Regulated by same mechanisms controlling Symp NS activity
- ∴ activation = ↑[catecholamine]
- ↑FoC
Thyroid Hormones
- Direct effects
- ↑FoC (↑Ca2+ uptake)
- Cardiac hypertrophy (↑protein synthesis)
- Indirect effects
- ↑symp stimulation
- ↑BMR
- Direct effects
Insulin
- Direct +ve INOTROPY of heart
- ∴Augmentation of glucose uptake
Temperature
- ↑temp = ↑HR
- ↑cardiac muscle membrane to ions → accelerate self-excitation
- Some ↑FoC but prolonged fever → exhausts metabolic system → cardiac failure
- ↓temp = ↓HR
Chemical
Oxygen
- Mod hypoxia → stimulates symp NS
- Severe hypoxia → myocardial depression
pH from ↑PaCO2
- ↓Ca2+ released when excited myocyte from SR
- ↓sensitivity of myofilaments to Ca2+
- Interference of actin-myosin interaction
Ca2+
- Hypocalcaemia = cardiac weakness
- Hypercalcaemia = spastic contraction
K+
- Hyperkalaemia = ↓RMP = ↓intensity of AP = weak contraction
- Bradycardia → blocks conduction through AV bundle