21B03: Exam Report
Discuss the physiological determinants of cardiac output
65% of candidates passed this question.
Although the pass rate for this question was reasonably high the examiners commented on a lack of detailed knowledge within most answers for such a core component of our daily practice. Several candidates failed to provide a normal value and only few provided anything other than 5l/min.
There was a general lack of detail, and at times, some confusion about the Frank Starling effect. Most candidates outlined the major determinants of stroke volume, although many were light on the determinants of each or incorporated incorrect facts. Several candidates did not mention HR as a determinant of CO
14A19: Exam Report
Define cardiac output. (10% of marks)Outline the factors that affect cardiac output. (60% of marks) Briefly describe the thermodilution method of measuring cardiac output.(30% of marks)
58% of candidates passed this question.
This is a core question. It was expected candidates could provide a definition (heart rate x stroke volume) and then move on to outline factors that affect it (afterload, preload, contractility). Additional marks were awarded for descriptions of the relationship to mean systemic filling pressure and other influences beyond this.
Most candidates described a thermodilution cardiac output curve but almost all described the technique as based on the “Fick equation or method” (which is used to estimate cardiac output from oxygen consumption). Very few candidates correctly identified the Stewart Hamilton equation as the integration method used to relate cardiac output (flow) to temperature change as an example of indicator dye dilution.
Candidates seemed to lack depth and understanding on this topic.
G6iii / 21B03 / 14A19: Define CO (10 marks). Outline the factors that affect CO (60 marks). Briefly describe the thermodilution method of measuring CO (30 marks)
Definition
- CO = HR x SV = volume of blood ejected by heart per minute
(normal CO = 5L/min in a 70kg male)
- Determinants of CO are HR and SV
Heart Rate
↑ HR = ↑CO
- Set by pacemaker cells of heart
- SA Node →high intrinsic frequency ~100bpm
- Basal vagal tone →∴normal HR ~70bpm
- Regulated by ANS →symp = ↑HR, parasymp. = ↓HR
- Influenced by electrolytes, pH, drugs
Stroke Volume = amount of blood ejected by heart per beat
- SV influenced by preL, afterL, contractility
Preload: load on myocardial fibres just prior to the onset of contraction →sarcomere length at the end of diastole
- ↑PreL = ↑CO
- 7 factors determining preload:
1. Venous pressure
- ↑Venous P = ↑venous return = ↑PreL = ↑CO
- Venous P depends on
- Total blood volume
- Gravity
- Muscle contraction
- Venous compliance
2. Ventricular compliance
- ↑C = ↑EDV = ↑CO
- ↑Compliance = ↑filling for any given pressure
3. HR
- ↓HR = ↑filling time = ↑EDV = ↑CO
4. Atrial contraction
- At rest atrial kick = 10% ventricular iflling
- With symp. stimulation = ↑FoC = 40% ventricular filling
- Atrial kick = ↑EDV = ↑CO
5. Inflow resistance
- ↑inflow R (tricuspid/mitral stenosis) = ↓EDV = ↓CO
6. Outflow resistance
- ↑outflow R (↑PAP/AoS) = impaires ventricle emptying = ↑EDV which will ↑PreL but outflow R will ↓CO↓
7. Ventricular inotropy
- Ventricle systolic failure = ↓emptying = ↑preL but ↓CO
Afterload: the sum of all factors required to overcome so that blood may be ejected from the heart to the arterial circulation
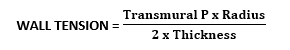
- AfterL gives rise to WALL TENSION in ventricle à∴AfterL can be thought of as the wall T required to overcome impedance to eject blood into the circulation
- ↑AfterL = ↓CO
- ∴Factors affecting afterload are:
- Factors affecting wall tension
- Factors affecting outflow
- Ventricle transmural P
- ↑transmural P (i.e. obstructed airway) = ↑wall T = ↑afterL = ↓CO
- Ventricle wall thickness
- ↑thickness = ↓wall tension = ↓afterL = ↑CO
- Ventricle radius
- ↑radius (cardiomyopathy) = ↑wall tension = ↑afterL = ↓CO
OUTFLOW affected by:
- SVR = R to blood flow by all systemic vessels
- Based on HP equation: R =
- ∴radius has greatest influence
- ∴↑radius = ↓R = ↓afterL = ↑CO
- Outflow tract resistance
- ↑resistance to outflow (i.e. AS) = ↑afterL = ↓CO
- Aortic root compliance
- ↓compliance = ↑afterL = ↓CO
Contractility = the intrinsic ability of myocardial fibres to shorten, independent of preL and afterL
- Contractility depends on:
- Substrate supply
- Integrity of myofilaments
- Coordinated electrical depolarisation
- Metabolic homeostasis
- Coronary BF
Thermodilution
- Thermodilution is a flow-based technique to measure CO
- Thermodilution techniques for CO measurement can be via:
- R) heart →PAC
- Transpulmonary →PICCO
Right Heart CO Measurement
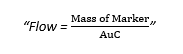
- CO measurement is based on the FICK PRINCIPLE
“Amount of indicator substance taken up over time = A – V difference of the substance x blood flow”
- This was originally tested with O2 consumption, but was difficult to measure, so thermodilution uses Temperature
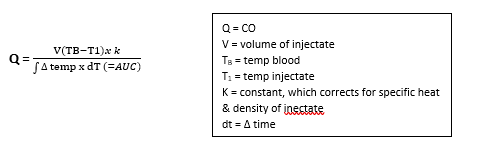
- Current thermodilution practice of measuring CO uses a modified STEWART HAMILTON EQUATION
- The marker is temperature
Steps
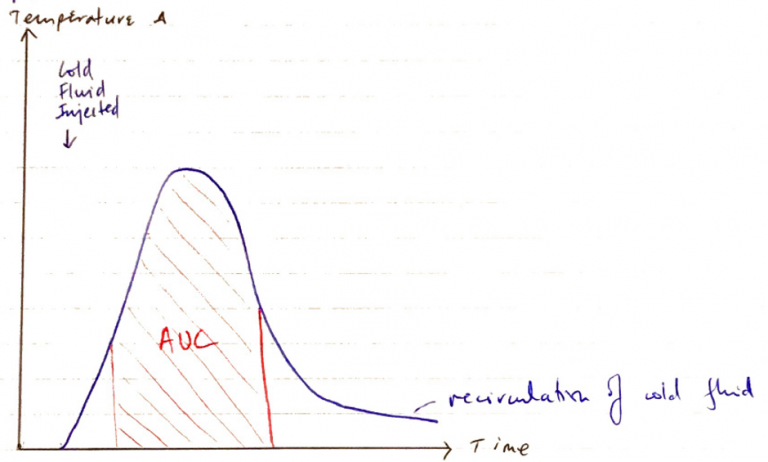
- Bolus of sterile solution (injectate) colder than pt blood is injected into RA port
- Injectate mixes with RA blood →TV →RV →PA
- Thermistor located 4cm from tip of catheter situated in PA detects ∆blood temp as blood passes catheter tip
- Temp ∆ detected produces a curve which shows: ∆TEMP vs TIME calculated by a computer & converted into a measurement of CO by S – H application
Limitations
Injection
PAC
Patient
Slow bolus
Inaccurate volume
Inaccurate temp
Malpositioned
Thermistor wedged
Resp fluctuations (should be measured in expiration)
TR
Hct
Arrythmias
Assumptions
- Constant flow
- Normal heart & valves
- No resp. fluctuations
Disadvantages
- Insertion of PAC is invasive
- Arterial injury
- PTx
- Chylothorax
- Nerve injury
- PA rupture
- Valve damage
Advantages
- Non-toxic indicator
- Repeated measurements easily
- Computer performs all patented algorithms