G6iii: Waveforms & pressures seen in each anatomical location during insertion of a PAC
Definition
PAC = the PAC is a balloon-tipped thermodilution catheter 110cm long, that is inserted via a large vein & floated into the PA
Indications
- Measure CO (via thermodilution)
- Central temperature monitoring
- Measure intracardiac pressures (CVP, RA RV, PA)
- Estimates LV preload (via Wedge Pressure)
- Sample mixed venous blood
Insertion
- Sterile Seldinger Technique
- Through a sheath into central vein
- Connected to a pressure transducer to ‘map/ your run
- Once RV waveform seen, balloon inflated to facilitate PAC progress through R) heart
- Once PA is reached, PCWP/waveform is used to confirm position
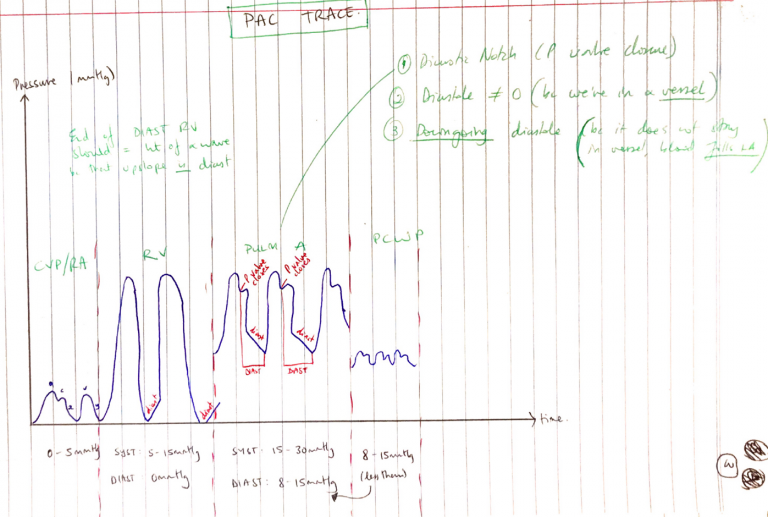
CVP/RA
- Pressure 0 – 5mmHg
- a wave = atrial contraction
- c wave = isovolumetric contraction
- x desc. = beginning of systole where RV pulls TV
- v wave = venous return (RA filling)
- y desc. = passive RV filling
RA
- Systole 15 – 30mmHg/Diastole 0mmHg
- Upstroke in diastole (filling)
- Systole without dicrotic notch
PA
- Systole 15 – 30mmHg/Diastole 8 – 15mmHg
- Dicrotic notch (pulm. valve closure)
- Downstroke diastole (because it’s a vessel & fills LA)
- Diastole ≠ 0 because we’re in a vessel
Pulmonary Wedge
- Estimates LVEDP & ∴ indicator of LVEDV (LV PreL)
- 5 – 15mmHg
- Should look like RA trace but massively overdamped ∴looks like a squiggly line
PCWP
- Wedging provides a static column of blood between PA & LA
- Allow estimation of LVEDP (and indicates LVEDV)
- Must be in WZ3
Confirming Placement
- In WZ3 below RA on XR
- Should not vary >50% with PEEP (because then Alveolar P is affecting it too much)
- PCWP should be less than diastolic P in PA
Measurements
Direct
RA pressure
RV pressure
PA pressure
PCWP
CO
Mixed venous oxygen saturation
HR
Indirect
CI
SV
SVI
SVR
SVRI
PVR
PVRI
CaO2 – arterial oxygen content
CvO2 – mixed venous oxygen content
DO2 – oxygen delivery
VO2 – oxygen consumption
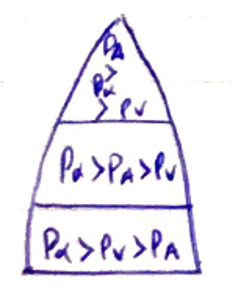
- RV diastolic must be lower than CVP, so RV can fill in diastole
- PCWP wave similar to CVP but higher
- PA diastolic must be higher than RV diastolic
- PA is a vessel, diastole ≠ 0
- PA diastole is down-going because it is a vessel, blood doesn’t stay there, it fills the LA
Pathology That Alters Valves
CVP/RA
- Fluid overload
- RV dysfunction
- TR/TS
- Tension/Tamponade
- Severe LV dysfunction/MV dysfunction
RV
- Pulmonary hypertension
- LV dysfunction (bulging LV septum)
- Tamponade
PAP
- Any cause of Pulmonary HTN
- Idiopathic
- Vasculitis
- Raised pulm. venous P
- Chronic lung disease
- Valvulopathies
PAWP
- Fluid overload
- PEEP/↑intrathoracic P
- Valvulopathies (MV)
Advantages
- Directly measure & indirectly derive wide range haemodynamic variables
- Non-toxic “indicator” (temperature)
- Extra lumens for drug administration
- Once inserted, can repeat measurements for trend/guide fluid therapy
Disadvantages
- No study demonstrate I/O PAC = improved clinical outcome
- Skilled operator
- Misinterpretation of data
- Many variables can make data inaccurate
Injection
Slow bolus
Inaccurate vol.
Inaccurate temp.
PAC
Malpositioned
Thermistor wedge
Patient
Resp fluctuations (should be measured at expiration)
TR
HCT
Arrhythmias
- Complications of catheter insertion → many are critical:
- Arrhyhthmias
- Knotting of catheter
- Balloon rupture
- PA infarction
- PA rupture
- Endocarditis
- Thromboembolism
- Air embolism
- Valve rupture