F4iii / 20B02 / 17B24 / 15B04: What is FRC and how is it measured
20B02: Exam Report
Define functional residual capacity (10% marks). Outline the functions (70% marks) of the functional residual capacity and the factors affecting it (20% marks)
79% of candidates passed this question.
This question was in two parts with the percentage of marks allocated an indication of the relevant time or detail expected per part. The second part of the question also contained two distinct headings which should have been used in the answer. As an outline question, dot points with a brief explanation of each point were expected. Most candidates drew diagrams, few of which added value. For a diagram to add value it should be accurate, have labelled axes, a scale with numerical values and units. As a general rule, diagrams should also be explained and help to illustrate or relate to a written point.
17B24: Exam Report
What is functional residual capacity (30% of marks)? Describe two methods of measuring functional residual capacity (70% of marks).
59% of candidates passed this question.
Most candidates could state 2 methods of measuring FRC. Some candidates (especially for nitrogen wash out) failed to provide enough information e.g. statements such as “if the amount of nitrogen is measured then FRC can be derived” were insufficient to score many marks.
15B04: Exam Report
What is functional residual capacity and describe how it is measured.
25% of candidates passed this question.
This question requested a definition AND a description of measurement (one method if correctly discussed could and did generate a pass mark) although additional marks were awarded if multiple measurement methods were mentioned or described. Detailed descriptions of the factors effecting FRC and its functions were NOT requested and scored no marks. “Fowlers method” uses 100% oxygen and nitrogen analysis to calculate anatomical dead space – NOT FRC – so scored no marks. Both Helium dilution and nitrogen washout (with 100%oxygen) enable calculation of FRC using C1V1=C2V2 where V2 = V1+FRC. Body plethysmography requires more complex calculations of P1V1= P2V2 (Boyles Law) applied twice = for the box and then the lung. Few candidates had a clear understanding of this method.
Most answers did not demonstrate the depth of understanding of the measurement techniques that was required to score highly.
F4iii / 20B02 / 17B24 / 15B04: What is FRC? How is it measured?
Definition
- FRC = volume of lungs at the end of normal tidal respiration
- Capacity = RV + ERV
- Normal FRC = 30mL/kg
Factors Affecting FRC
- Height: ↑ with ↑weight
- Weight: ↑ with ↑lean weight
- Sex: F have 10% less FRC for same weight
- Abdominal Pressure
- Supine → ↓FRC due to abdomen contents pushing diaphragm up by 4cm
- Obesity → ↓FRC
- Pregnancy → ↓FRC
- Chest wall restriction
- Any restriction to chest expansion e. burns = ↓FRC
- Lung disease
- ↑FRC with ↑elastic recoil (emphysema)
- ↓FRC with ↓elastic recoil (restrictive lung disease)
- Muscle paralysis & anaesthesia
- Anaesthesia does not ∆FRC in sitting position
- Supine patient → GA +/- paralysis will lose muscle tone of diaphragm → abdo contents push up → ↓FRC
- Occurs in first few mins of anaesthesia
- FRC does not return to normal until some hrs post-op
- ↓FRC will bring end expiratory vol closer to RV & even below CC (esp elderly) → airway collapse & atelectasis
Functions of FRC
- O2 store: major body O2 store which can be significantly ↑by pre-O2
- Buffer PaO2: continuous O2 supply prevents PaO2 swings in ventilatory cycle
- Minimises airway closure:
→ Minimises V/Q mismatch → if volume where INSP starts > CC, this minimises airway closure which minimises shunting
→ Prevents atelectasis (small airway closure during expiration when CC > FRC)
- Minimises WoB: FRC on steep part of compliance curve → minimises WoB
- Minimises PVR: PVR minimal at FRC
3 Methods Used to Measure FRC
1. Helium Wash-in Technique
- Closed circuit system
- He is not absorbed by blood
- Amount of helium is known = Concentration x Volume
- Patient breathes normal breaths to measure FRC & end of maximal expiration to measure RV
- Helium in lung & spirometer equilibrate
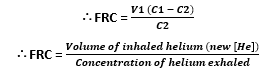
- Concentration before & after is C1V1 = C2V2
- C1 = initial known [helium]
- V1 = volume of gas in spirometer
- C2 = final [helium]
- V2 = total gas volume (FRC + volume of spirometer)
2. Nitrogen Washout Technique
- C1V1 = C2V2
- N2 in atmosphere 79%
- This sits in FRC & not absorbed
- FRC washed out of lung by breathing 100% FiO2
- Amount of N2 removed is used to calculate FRC
- C1 = [Nitrogen] at start of test
- V1 = FRC
- C2 = [Nitrogen] of exhaled volume
- V2 = total exhaled volume during 7 minute (washout) breathing
NB: Gas dilution methods only measure communicating gas volume & will not include gas trapped behind obstructed airways or PTX
N2 Washout
- Initial FRC [N2] 80%
- Total N2 volume washout = 4L
- ∴Initial lung volume (FRC)
= 4L/0.8
= 5L
He Washin
- 50mL the introduced
- Final [ ] He 1%
- ∴lung vol = 50mL/1%
= 5L
3. Body Plethysmograph
- Application of Boyle’s Law
- Boyle’s Law: P x V = constant
- Patient sits in glass tight box
- Breathes against a shutter (in a mouth piece)
- Box pressure → ∆box pressure = ∆lung volume
- Mouth pressure → ∆ mouth pressure = ∆ alveolar pressure
- Volume of Box is known
- Double application of Boyle’s Law to calculate FRC
NB: Body plethysmography can calculate the gas trapped within lung distal to closed airways
∴in normal lungs FRC values of Plethysmography & dilution not much different, but may be in airway disease
- Author: Krisoula Zahariou