F8iv / 15B23: Describe the factors that affect the partial pressure of CO2 in mixed venous blood
15B23: Exam Report
Describe the factors that affect the partial pressure of CO2 in mixed venous blood.
15% of candidates passed this question.
It was expected candidates would define key concepts, particularly ‘mixed venous’. Many candidates knew some of the elements that contributed to mixed venous PCO2 but few described all of the main factors. There was little mention of tissue capillary flow as a factor
affecting mixed venous CO2.
F8iv / 15B23: Describe the factors that affect the partial pressure of CO2 in mixed venous blood
Definitions
Mixed venous pCO2 (PvCO2): The partial pressure of carbon dioxide in mixed venous blood taken from the pulmonary artery using a PAC. Blood is “mixed” in the right ventricle and is representative of blood from the whole body (including the coronary sinus).
Normal PvCO2 = 45-50mmHg
Partial pressure of CO2 is dependent on:
- CO2 content of mixed venous blood (CvCO2)
- Position of the CO2 dissociation curve
CO2 Content of Mixed Vvenous Blood
CvCO2 – can be explained using a modification of the Fick Equation:
- VCO2 = CO(CvCO2 – CaCO2)
- \( \text{CvCO2 = CaCO2 + } \frac{\text{ VCO2 }}{\text{CO}} \)
- Therefore, CvCO2 is further influenced by:
- Cardiac Output – decrease -> increased CvCO2
- In low flow states, more CO2 is added to capillary blood due to increased transit time
- VCO2 (CO2 production) – increase -> increased CvCO2
- CO2 is produced within the Citric Acid Cycle (CAC) in the process of aerobic metabolism
- VCO2 is dependent on the metabolic rate and the delivery of O2 to the tissues to allow aerobic respiration
Factors causing increased VCO2:
- Increased aerobic metabolism (e.g. exercise, Fever/↑ temp)
Factors causing decreased VCO2:
- Anaerobic metabolism (e.g. poor oxygen delivery to tissues, inability to utilise O2)
- CaCO2 (arterial CO2 content) – increase -> increased CvCO2. This is in turn influenced by the balance between:
- PaCO2 and Alveolar Ventilation (VA)
- \( \text{PaCO2 = } \frac{\text{ k }}{\text{VA}} \)
- Therefore, as VA increases – CvCO2 decreases.
- VA is tightly controlled through negative feedback – PaCO2 is the most important stimulus for controlling VA.
- Sensors: Central and peripheral chemoreceptors
- Integrator: Brainstem respiratory centres
- Effectors: The muscles of respiration
- Factors increasing VA:
- PaCO2 and Alveolar Ventilation (VA)
- CaCO2 (arterial CO2 content) – increase -> increased CvCO2. This is in turn influenced by the balance between:
- ↑PaCO2
- ↓ PaO2
- ↓ pH
- ↓ Blood pressure
- ↑ core temperature
- Pain
- Pregnancy
- Exercise
- ↓ BSL
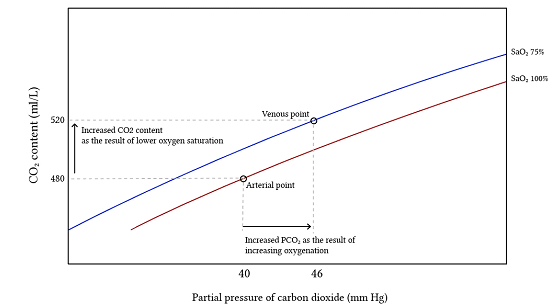
The CO2 Dissociation Curve
The mixed-venous CO2 dissociation curve is left-shifted relative to the arterial curve, due to the Haldane Effect: deoxygenated blood has an increased CO2 carrying capacity. This is due to:
- Deoxygenated haemoglobin
- Increased ability of deoxy-Hb to form carbamate compounds
- Increased ability of deoxy-Hb to bind H+ ions, allowing more CO2 to form HCO3-
- Erythrocyte Chloride Shift (Hamburger Effect)
- The exchange of HCO3 and Cl in RBCs – allows more CO2 to form HCO3, catalysed by RBC carbonic anhydrase
- Deoxygenated haemoglobin
Mixed venous oxygen saturation (SvO2) is typically 60-80%. A lower SvO2 -> greater degree of left shift of the CO2 dissociation curve -> lower PvCO2 for a given CvCO2.
Reference: Deranged Physiology
Author: Joshua McLarty