F8i / 16A01 : Outline the determinants of O2 delivery to the tissues
16A01: Exam Report
Outline the determinants of oxygen delivery to the tissues.
61% of candidates passed this question.
An opening statement such as oxygen delivery = cardiac output x oxygen content then allowed a more detailed description of the determinants of both oxygen content and cardiac output. It was expected candidates could detail the formula for Oxygen Content = Sat O2 % x 1.34 x Hb x 10 (depending on units) + PaO2 x .003, or x .03 (units) and accurately describe each element. Determinant of cardiac output completed the answer, often starting with CO = HR x SV while discussing the importance of preload, afterload and contractility.
Many candidates spent little time on cardiac output which cost valuable marks. Some candidates provided a lot of detail on how oxygen is managed within the lung, the majority of which was not required as part of the answer. Some candidates answered the question
describing the oxygen cascade only which was not sufficient to score well.
F8i 16A01: Outline the determinants of O2 delivery to the tissues
- Oxygen flux (refers to) = the rate of O2 delivery to the peripheral tissues
- O2 flux = Oxygen content of blood x CO
O2 Flux (mL/min) = oxygen content blood (g/dL) x CO (mL/min)
Oxygen Content = oxygen bound to Hb + Dissolved O2
= ([Hb] x SpO2 x 1.34) + (PO2 x 0.003)]
CO = HR x SV
Oxygen Content
[Hb] x 1.34
- Oxygen binds reversibly to Hb: Hb + O2 ⮂ HbO2
- Huffner’s Constant = max amount of O2 that can be carried by 1g Hb
- Normal adult Hb (g/dL) = 15
∴O2 capacity for Hb = 15 x 1.34 = 20.1mL O2/100mL blood
SpO2
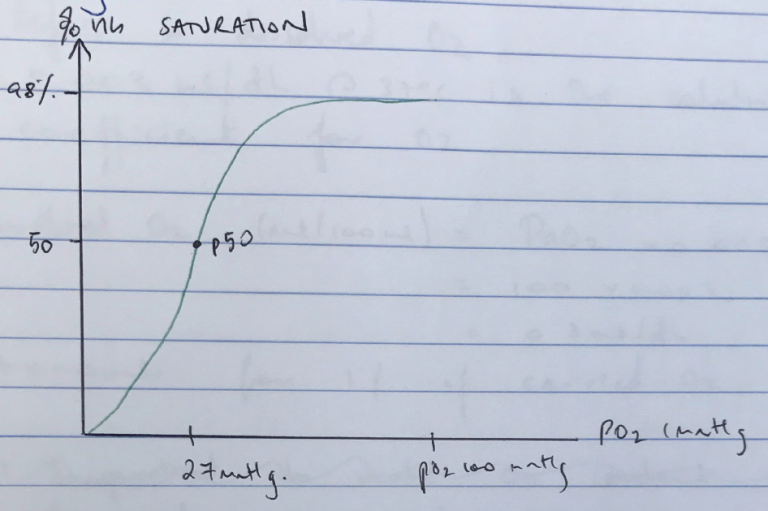
- ODC describes relationship b/w PO2 & % SATURATION OF Hb with O2
- Oxygen saturation is how much Hb is combined with O2 vs how much can actually bind → x 100 to give %
- Saturation of Hb with O2 in arterial blood is 97.5% for PO2 100mmHg
- KA ARTERIAL POINT of ODC
- ODC is sigmoid-shaped due to +VE COOPERATIVITY
- Affinity of O2 is lowest before first molecule binds Hb in its ‘TENSE’ state
- Then as subsequent O2 binds (4 per Hb), affinity ↑
- At PO2 > 60mmHg the curve plateaus so that Hb % saturation is minimally affected by altering PO2
- Different factors can ↑/↓ Hb affinity for O2 & ∴O2 delivery
- ∴P50 is used as a reference point
R) → ODC → ↓ Hb Affinity
↑2,3 DPG
↑CO2
↑Temp
↓pH
L) → ODC → ↑ Hb Affinity
↓2,3 DPG
↓CO2
↓Temp
↑pH
- The BOHR EFFECT = ↓O2 affinity at low pH & ↑O2 affinity at ↑pH
- Important because it offloads O2 to metabolically challenged areas
PO2 x 0.003
- Refers to dissolved O2
- 003mL/dL @ 37°C is the solubility coefficient for O2
- Dissolved O2 (mL/100mL) = PaO2 x 0.003
- = 100 x 0.003
- = 0.3mL/dL
- Accounts for 1% of carried O2
Cardiac Output
- CO = HR x SV
- HR = resting HR is 60 – 100bpm
- ↑/↓ HR will affect time for diastole & ∴preload
- e. ↑HR = ↓diastole time = ↓preload = ↓CO
- Stroke volume is determined by: preL, afterL, contractility
PRELOAD: load on myocardial fibres prior to contraction = initial fibre length of a sarcomere
- Not able to measure in intact heart
- LVEDV used as a surrogate
- ↑preL = ↑fibre length = ↑force of contraction = ↑SV as per the FRANK STARLING MECHANISM → which will ↑O2 flux
AFTERLOAD: the sum of all factors that oppose LV ejection
- 5 factors affecting AfterL:
- Wall tension
- Ventricle outflow tract
- Vessel Root Compliance
- Root pressure
- Vascular resistance
- Wall tension is the most important determinant of afterL & in fact afterL is also KA the Wall Tension required to overcome impedence to ejection of blood in arterial circulation
- Because ventricle is a sphere it obeys LAW OF LAPLACE
(* Transmural P = Intraventricular P = Intrapleural P)
- Any ↑afterload will ↓CO & ↓O2 flux
- Contractility = the intrinsic ability of cardiac fibres to lengthen & shorten independent of PreL & AfterL
↑ Contractility = ↑ SV = ↑ CO = ↑ O2 Flux
Summary
- O2 Flux (mL/min) = CO x (([Hb] x 1.34 x SpO2) + (pO2 x 0.03))
= 50 x [(15 x 1.34 x 100) + (100 x 0.003)]
= 1000mL/min
→ 4 x the resting O2 consumption of 250mL/min
→ Tissues extract 250mL O2 (25%) and return 750mL to R) heart → accords with mixed venous O2 SpO2 of 75%
→ IMPORTANT: O2 delivery is product of 3 variables and 1 constant (1.34)
- CO
- [Hb]
- SpO2
→ If one variable ↓50%, delivery ↓
→ If all 3 variables ↓we may not be meeting resting O2 consumption
→ That is why all variables: CO, [Hb], SpO2, must be optimised for adequate O2 FLUX
- Author: Krisoula Zahariou