Q2i / 16A10 / 15A08: Pharmacology of warfarin
16A10: Exam Report
Outline the pharmacology of warfarin.
61% of candidates passed this question.
The “traditional” pharmacology answer structure was useful to avoid omitting key details. Warfarin is a synthetic coumarin derivative presented in tablet form for oral use . It is a racemic mixture. S-enantiomer is 2-5 times more potent than the R-enantiomer. It is used for anticoagulation and the usual dosing involves a loading dose ( 3 to 5 mg for 1 to 3 days) then maintenance dose titrated to INR. It was expected answers would then detail mechanism of action, absorption (commenting on bioavailability), distribution, elimination, excretion and adverse effects. Warfarin has contraindications in pregnancy being teratogenic in first trimester and increasing the risk of fetal haemorrhage in third trimester.
Better answers provided increased detail on mechanism of action including the initial procoagulant effect due to protein C and S inhibition and some details about monitoring effect with INR / PT.
Warfarin has several important drug interactions and detailing these gained additional marks. Additional credit was given for discussion of reversal options, which includes 1) Stop administration – days 2) Prothrombinex – hours 3) FFP – hours 4) Vitamin K depends on dose given.
15A08: Exam Report
How does warfarin exert its anti-coagulant effect (50% of marks)? Outline the pharmacology of the agents that can be used to reverse the effects of warfarin, giving examples (50% of marks).
38% of candidates passed this question.
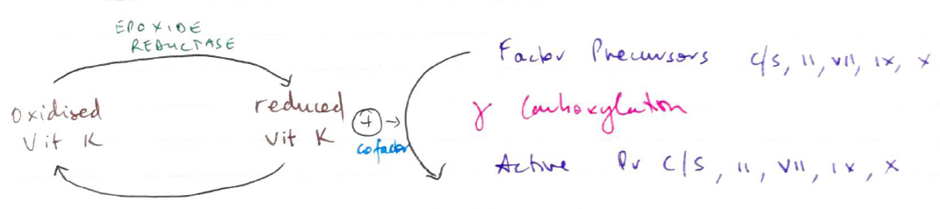
Warfarin is a competitive inhibitor of the enzyme vitamin K epoxide reductase which converts oxidised or inactive vitamin K to reduced or active vitamin K Reduced vitamin K is required for the gamma carboxylation of the glutamate residues in the vitamin K dependant factors (II, VII, IX and X) and proteins C and S. This gamma carboxylation converts these clotting factors from their inactive to their active form resulting in coagulation. The presence of warfarin inhibits this conversion process resulting in anticoagulation. The presence of inactive protein C and S explains the initial hypercoaguable effect of warfarin.
The three main agents used to reverse the effects of warfarin are vitamin K, prothrombinex and fresh frozen plasma (FFP). It was expected answers would provide a brief overview of all three agents. Most candidates did not highlight the fact that parenteral vitamin K requires a few hours to work whereas prothombinex and FFP work immediately.
Better answers noted additional facts such as oral vitamin K because it is fat soluble requires the presence of bile salts to be absorbed from the gut or the rare but life threatening hypersensitivity reaction caused by intravenous vitamin K possibly related to its preservative benzyl alcohol.
A common omission was the amount of coagulation factors in international units (IU) in an ampoule of prothormbinex or the dose required to reverse warfarin anticoagulation. A description of the clinical pros-cons of the various agents was not required to answer the question.
Q2i / 16A10 / 15A08: Outline the pharmacology of warfarin
Chemical
Synthetically derived coumarin anticoagulant
NB: coumarin is a chemical in many plants
The term comes from the French ‘tonka bean’ = COUMAROU, from where coumarin was first isolated
Use
- Prevent emboli in AF, value disease, prosthetic valves
- Tx DVT/PE
Presentation
Oral tablets 1 – 10mg
Racemix mixture
S-isomer x 4 potent
Dose / Route
5 – 10mg OD orally for 3 days
→ Daily bloods
→ Then alternate days for 1/52
→ Then fortnightly
Heparin should be overlapped for 48hrs if patient has active thrombus
Target INR
AF 2 – 2.5
Prosthetic valve 2.5 – 3.5
All else 2 – 3
Onset
8 – 12hrs onset
- Warfarin halts production of new clotting factors
- No effect on already active factors
∴requires hours for full effect (for all of those factors to be degraded) → mainly F II (PRO THROMBIN)
DoA
Half lives:
of Protein C/s → 7 → 9 → 10 → 2
= 7 6 24 40 60hrs
DoA → effects last 2 – 5 days (life of clotting factors)
Very slow clearance 3mL/kg/min & new clotting factors need to be synthesised
MoA (mechanism)
- Inhibits production of Vit K dependent clotting factors & proteins
- Vit K is required to synthesise:
- 4 clotting factors: II, VII, IX, X (TV channels)
- 2 anticoag proteins; Pr C & S
- Formation of these requires y-CARBOXYLATION
- Reduced Vit K (as cofactor)
- Warfarin inhibits EPOXIDE REDUCTASE. This enzyme reduces oxidised Vit K so it may be used again
∴ no cofactor for carboxylation → ↓ synthesis clotting factor & protein
PK
A
High lipid solubility
100% OBA
Rapid absorption
Peak plasma 4h
D
99% PPB (albumin)
VD 0.1L/kg
Small due to high PPB
M
Entirely by liver
Phase 1 & 2 reaction
CYP450
Metabolites then conjugated & glucoside
E
Metabolites excreted in urine & faeces
t ½ = 40hrs prolonged
Predictability
Highly variable
- VIT K AVAILABILITY
- Diet
- ↓synthesis
- ↓absorption (requires bile salts)
- Albumin alters Vit K absorption
- LIVER DISEASE
- ↓synthesis clotting factors
- Altered metabolism of warfarin
- METABOLISM
- Fever/hyperthyroid → ↑breakdown coag factors
- Myxoedema → ↓breakdown coag factors
- DRUG INTERACTIONS
Susceptible due to high PPB & sole liver metabolism
Enhanced Effect
NSAIDs/Aspirin (high PPB)
EtOH → prolongs clearance
Other PPB competitors
- Amiodarone
- Cimetidine
- Metronidazole
Erythromycin
Decreased Effect
Liver enzyme inducers
- Barbituates
- OCP
- Phenytoin
Rifampicin
Adverse Effects
- Bleeding (nose, urine, head, menstrual, GI etc)
- Teratogenic → crosses placenta
- Cutaneous necrosis → may occur in patients with ↓activity of Pr C
Monitoring
Warfarin is reported by monitoring INR, which is the Prothrombin Time (ext & common pathway) according to International Reference Thromboplastin
Reversal
- Cease warfarin! – requires new clotting factors to be synthesised so will require replacement with:
- Vitamin K – replenish stores, days to take effect
- FFP – immediate effect, however requires group specific matching and thawing
- Prothrombinex – requires Haem approval, immediate factor replacement
- Activated FVII
- Author: Krisoula Zahariou