K1ii / 22A10 / 18A15 / 16B18 / 16A14: Determinants of ICP
22A10: Exam Report
Discuss the determinants of intracranial pressure (80% marks) and outline how it can be measured (20% marks)
64% of candidates passed this question.
In the good answers to this question, and there were a number, the candidates included the volumes of the cranium and a correct description of the Monroe Kellie doctrine.
A good answer should have included the compensations and consequences of increases in intra-cranial volumes; a discussion of all three components (brain tissue, blood, and CSF) and how they affect intracranial pressure; and then information on intra-ventricular and parenchymal devices in measuring ICP, briefly including their pros and cons.
A common issue was writing quite a lot more than was needed on the relationship of cerebral blood flow to cerebral blood volume, and/or on the physiological consequences of raised ICP, which seemed to leave little time for discussion elsewhere.
A few candidates did not provide any response for ICP measurement (worth 20% of the marks). Few candidates provided the intra-cranial elastance equation. A significant proportion of candidates missed out a part of the question, either the factors that affect CBV or ICP measurement.
18A15: Exam Report
Describe the physiological regulation of intracranial pressure.
45% of candidates passed this question.
A definition and a normal value were expected. A description of the Monro-Kellie doctrine was expected. Better answers divided into the various components of the cranium with the answer focussing on cerebral blood volume and CSF volume as the brain tissue as no capacity to change its volume.
16B18: Exam Report
Discuss the determinants of intracranial pressure (80% of marks). Outline how it can be measured (20% of marks).
55% of candidates passed this question.
It was expected answers would include an explanation of the Monro-Kellie Doctrine. Many candidates gave insufficient details of compensatory mechanisms especially regarding decreased total cerebral blood volume (primarily venous) in response to increased intracranial pressure.
Most candidates had all the information but had difficulty synthesising the information to write a cohesive answer. Factors affecting ICP could be divided into factors affecting CBV, factors affecting CSF and factors affecting brain tissue. Under factors affecting CBV the effect of blood gases, autoregulation, temperature, metabolism, drugs and venous obstruction could have been detailed.
16A14: Exam Report
Describe the factors that influence intracranial pressure
69% of candidates passed this question.
A structure approached works well for “describe the factors …” questions. Better answers provided a definition of ICP, explained the Monro-Kellie doctrine and then detailed the factors which affect the volume of each of the components – cerebro spinal fluid (CSF), cerebral blood flow and brain parenchyma. Some candidates focused only on factors which cause intracranial hypertension and were thus unable to score full marks. Many candidates stated that CSF production was ICP dependant which is incorrect.
K1ii / 22A10 / 18A15 / 16B18 / 16A14 : Discuss the determinants of intracranial pressure (80 marks) + Outline how it can be measured (20 marks)
Definition & Normal Values
- ICP = the pressure inside the cranial vault
- Normal = 5 – 15mmHg
Determinants of ICP
- Pressure inside fixed vault is exerted by a fixed volume of:
- Brain tissue (80% volume)
- CSF (5% volume)
- Blood (10% volume)
- ICP is determined by total volume of each
- ICP also directly related to intrathoracic pressure as hit displays respiratory swing (ICP↑ coughing/straining/PEEP)
- ICP is important because it determines CPP
CPP = MAP – ICP
Monroe-Kellie Doctrine
- Skull is rigid box
- Fluids are incompressible
- M-K states that any ↑component of cranium must be met with equal ↓another component of cranium, for ICP to remain normal
Factors Affecting CBV
- CBF = 750mL/min
- CPP = MAP – CVP
- An ↑ICP will create a Starling Resistor whereby ICP > CVP ∴CPP = MAP – ICP
- ∴↑CBF = ↑ICP
- Autoregulated b/w 50 – 150mmHg
- Coupled to CMRO2
- ↑linearly with ↑PaCO2
- ↑exponentially with ↓PaO2
- ↑with venous congestion/obstruction
- Affected by drugs i.e.:
- PPF = ↓CMRO2 → ↓CBF → ↓ICP
- Ketamine → ↑CMRO2 → ↑CBF → ↑ICP
Factors Affecting CSF
- 550mL formed daily by EPITHELIAL CELLS
- 2 places:
- 70% CHOROID PLEXUS of 2 lateral ventricles
- 30% EXTRACHOROIDAL – endothelial cells lining brain capillaries
- Formation affected also by:
- Body Temp = ↓temp = ↓CMRO2 = ↓CSF
- ↑Serum osmolarity – ↓CSF
- Drugs ie Acetazolamide = ↓CSF
- Absorption → by ARACHNOID VILLI → Dural Sinuses
- Absorption affected by ICP
- ↑ICP = ↓CPP < 70mmHg = ↓CSF
- ↓ICP < 7mmHg = minimal CSF reabsorption
- Normally, formation = reabsorption
- Any ↑CSF production/↓CSF absorption = ↑ICP
Factors Affecting Brain Tissue
- Made of ICF & ECF
- ↑with brain occupying lesion
- ↑with cerebral oedema
- Any ↑brain tissue → ↑ICP
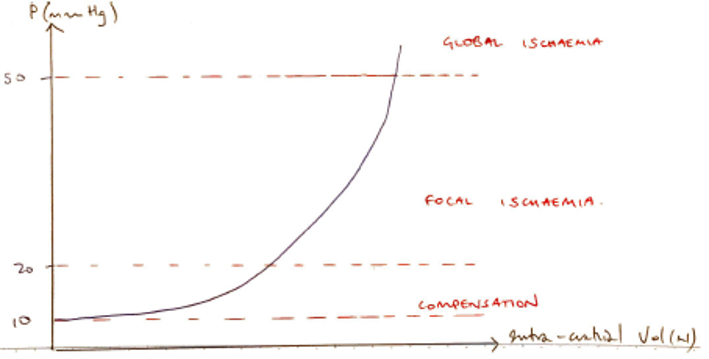
Consequence of ↑ ICP
- Due to ↑volume of components (CSF, blood, brain tissue)
- Initial compensation → CSF moves into spinal canal
- ↑CSF absorption & ↓CSF production
- Compression of venous sinuses → ↓intracranial blood vol
- As ↑↑↑ICP → CPP is compromised & cerebral ischaemic ensues
- Ischaemic of Medulla Vasomotor Centre → MASS SYMP D/C to improve perfusion (↑HR, ↑BP)
- Initially → headache, nausea, vomiting, papilledema, ↓GCS
- Eventually → herniation
↓
Brainstem forced out of Foramen Magnum
↓
Stretches CNS
↓
↑BP + ↑RR + ↓HR
KA CUSHING’S REFLEX (pre-terminal)
↓
Inability to sustain Cushing’s Reflex results in ↓BP, apnoea, fixed & dilated pupils
↓
Death
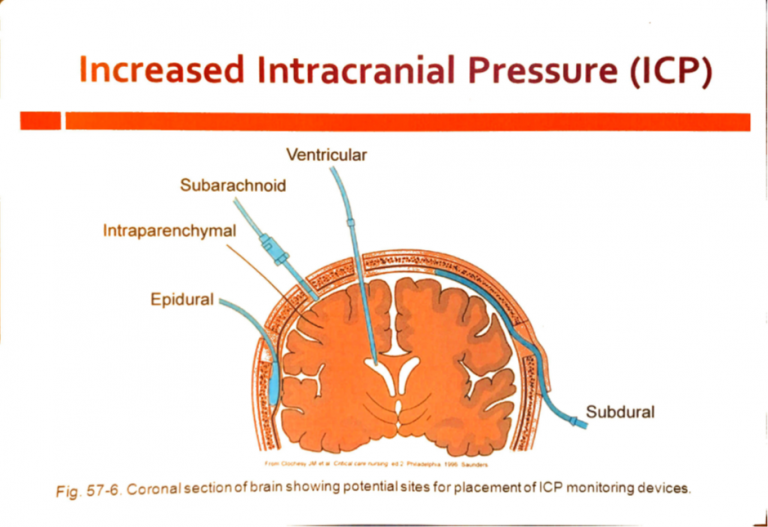
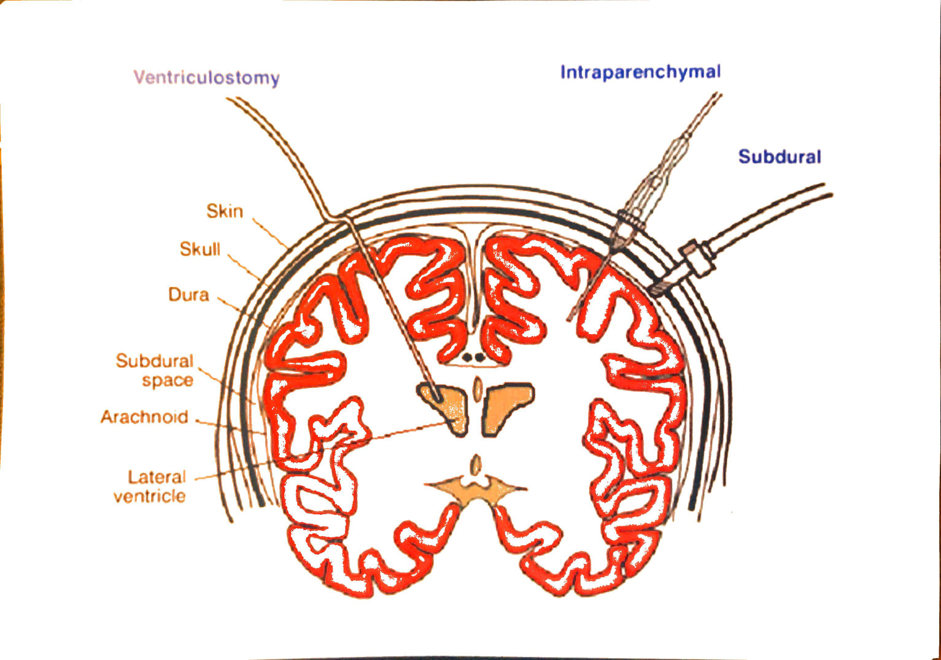
Measurement of ICP
Invasive
- Extraventricular drain → gold standard
- Parenchymal catheter
- Extradural ICP monitor
Non-Invasive
- Transcranial Doppler US
- Tympanic membrane displacement
- Optic nerve sheath diam
- Fundoscopy & papilledema
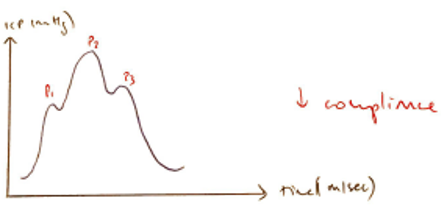
Oscillating Pressure Curve
- Progressively ↓P1, P2, P3 notches indicating propagation of cardiac pulse pressure
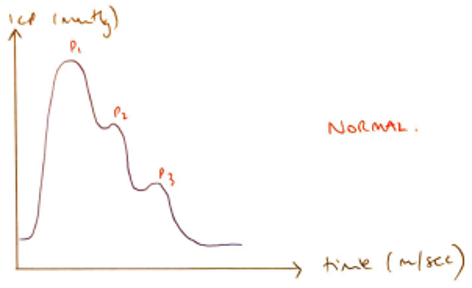
- P1 → PLEXUS PULSATIONS: arterial pulse transmitted through choroid plexus
- P2 → TIDAL WAVE: cerebral compliance, reflection of arterial pulse bouncing off brain parenchyma
- P3 → DICROTIC WAVE: closure of AV valve. If P1 > P2 = ↑ICP
Invasive
Extra Ventricular Drain
- Catheter tip passes through brain tissue
- Tip sits in Lateral Ventricle via Burr Hole
- Distal end connects to P transducer & drain system → allows drainage of CSF
- Zero level → external auditory meatus
- Can be recalibrated any time
- Monitors ICP cont & intermittent drainage
Codman Monitor
- Catheter tip lies in brain tissue
- Strain gauge tipped catheter of fibreoptic device
- Monitors ICP
- No recalibration possible after placement
Extradural ICP Monitor
- As per Codman but does not penetrate dura
Non-Invasive
Transcranial Doppler Ultrasonography
- US applied to MCA to measure BF
- Pulsatility index correlates with ICP
- Requires training & regular repetition
Tympanic Membrane Displacement
- CSF communicates with perilymph
- Based on:
- Stapedial reflex
- Patent cochlear duct
- Stimulation of Stapedial reflex
- Tympanic membrane movement correlates with ICP
- High Cochlear Fluid P = inward displacement TM
- Low Cochlear Fluid P = outward displacement TM
Optic Nerve Sheath Diameter
- Optic n = part of CNS
- Covered with Dural Sheath
- Small SUBARACHNOID SPACE b/w sheath & white matter
- ↑ICP = ↑sheath size
- Measure with trans-ocular US
- Correlates with ICP
Fundoscopy / Papilloedema
- Papilledema is due to ↑ICP
- Graded by FROSSEN Scale
- Usually done to screen patients with suspected ↑ICP
Measurement of ICP
Invasive
- Extraventricular drain → gold standard
- Parenchymal catheter
- Extradural ICP monitor
Non-Invasive
- Transcranial Doppler US
- Tympanic membrane displacement
- Optic nerve sheath diam
- Fundoscopy & papilledema
- Author: Krisoula Zahariou