N1iii / 16B13: Anatomy physiology of blood flow
16B13: Exam Report
Outline the anatomy and physiology of liver blood flow (60% of marks). Explain the changes to drug metabolism when liver blood flow decreases (40% of marks).
55% of candidates passed this question.
A statement regarding the quantum of hepatic blood flow with recognition of the contributions made by the Hepatic Artery and Portal Vein, drainage into the sinusoids before entering the hepatic vein which drains into the IVC would have been a good start. Discussion was then expected to revolve around how the liver blood flow is controlled. Answering this with respect to intrinsic and extrinsic factors along with an understanding of the semi-reciprocal relationship between hepatic arterial and portal venous blood flow would have rounded out a good answer to the first part of the question.
The second part of the question required recognition that hepatic clearance is the product of hepatic blood flow and the hepatic extraction ratio and considering the impact on drugs with a high or a low extraction ratio.
Many answers failed to adequately mention how hepatic blood flow was controlled/regulated thus limiting the marks available. Similarly, in the second part of the question, many candidates spent considerable time mentioning the principals of drug metabolism rather than focusing on the question asked.
The concept of hepatic drug clearance as the product of blood flow and its extraction ratio was poorly appreciated.
N1iii / 16B13: Outline anatomy & physiology of liver blood flow (60 marks). Explain the changes to drug metabolism when liver flow decreases (40 marks)
- Liver = largest visceral organ in body
- 25% CO
- 1.5L/min
- Dual vascular supply → HEPATIC A. & PORTAL V.
Hepatic Artery
- From Common Hepatic a. ← Coeliac Trunk
- 30% HBF
- 50% O2 supply (SpO2 98%)
- Pressure similar to systemic circulation
- Pressure in arterioles = 35mmHg
- Innervated ∴can constrict & dilate
Portal Vein
- From SMV, IMV, Splenic veins
- 70% HBF
- 50% O2 supply
- During fast ~85% SpO2 (this ↓ with ↑ gut activity)
- Low pressure 5 – 10mmHg
Functional Anatomy of Liver Blood Flow
Hepatic A Portal V
↓
Hepatic Sinusoids (2mmHg)
↓
Hepatic V
↓
IVC (0-2mmHg)
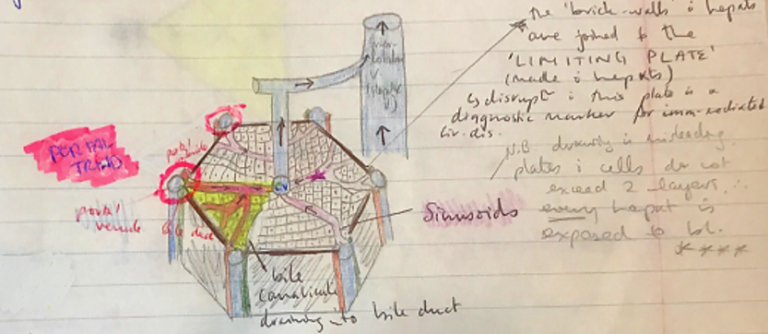
- Functional unit of liver → LIVER LOBE, a hexagonal structure consisting of plates of hepatocytes
- Hepatocyte plates radiate out from CENTRAL VEIN
- In each corner is a PORTAL TRIAD
- Hepatic a. (O2 blood)
- Portal v. (nutrient rich)
- Bile duct
Btw hepatic plates are SINUSOIDS (leaky caps) where blood from both HEPATIC A. & PORTAL V. percolates through to empty in CENTRAL V. → HEPATIC INTERLOBULAR V. → IVC
- Kupffer Cells (star-shaped macrophages) remain permanently in sinusoids & remove Ag’s & worn out RBC
- Secreted bile flows through BILE CANALICULI between adjacent hepatocytes towards bile ducts of triads
- Bile flow is in opposite direction to blood flow
- Bile exits liver via COMMON HEPATIC DUCT which empties into DUODENUM
NB: ‘Liver parenchyma’ is essentially anastomosing liver cell plates
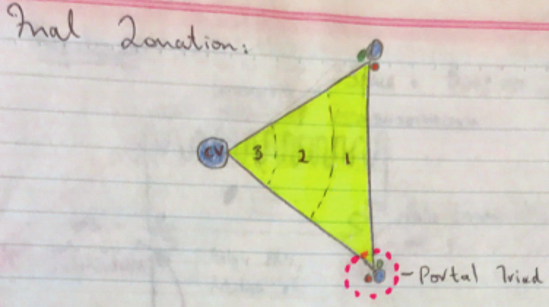
- 3 zones: differ in enzyme activity + physiological functions
- Zone 1: Periportal
- PO2 65mmHg
- Oxidative E-metabolism
- Gluconeogenesis, b-oxidation, cholesterol synthesis
- Urea synthesis (majority)
- Zone 2 → Intermediary
- Attributes of both zone 1 + 3 cells
- Zone 3 → Centrilobular
- Affected more by drug toxicity, vulnerable to ischaemic
- PO2 35mmHg
- Glycolysis, lipogenesis (don’t require much O2)
- CYTP450 drug detoxification – high [P450 enzymes]
- Zone 1: Periportal
NB: Toxicity depends on the toxin;
Zone 1: is the first area to be exposed to toxins – so if it directly injurious it will cause injury to periportal region (viruses)
Zone 3: Toxins requiring bioactivation (paracetamol) will cause centrilobular injury since ther eis a higher concentration of biotransforming enzymes
Regulation of Hepatic Blood Flow
INTRINSIC
EXTRINSIC
Hepatic arterial
Buffer response
Metabolic
Autoregulation
Neuronal
Humoral
Intrinsic
Autoregulation
- Pressure flow autoregulation allows constant BF despite fluctuating BP
- Only exists in HEPATIC A.
- Myogenic response of vascular smooth m. to stretch
- ↑systemic arterial P = ↑ transmural P = ↑myogenic tone (VC)
- ∴prevents ↑BF which would have occurred & vice versa
Metabolic
- ↓PaO2 & ↓pH Portal V = ↑Hep A flow
- Post prandial =↑osmolarity = ↑Hep a. & Portal v. flow
Hepatic Arterial Buffer Response
- Equilibrium b/w Hep a. & portal v. to maintain overall constant flow to liver
- ↑flow portal v. = ↓flow hep a. (vice versa)
- ?due to [Adenosine]
- Adenosine = produced by metabolism at constant rate
- ↓portal v. flow = adenosine accumulates = ↓arteriolar R = ↑Hep a flow
- ↑portal v. flow = adenosine washed away, ↑Hep a R = ↓Hep a. flow
- @maximal capacity HABR can double arterial flow
Extrinsic
Neural
- Vagus, phrenic, splanchnic n’s enter liver @ hilum
- SNS → regulation of Splanchnic
- Innervated terminal arterioles & venules
- ↓symp tone = ↑splanchnic reservoir volume
- ↑symp tone = hepatic blood volume transfer to central circulation
Humoral Control
- Hepatic a: VC (α1, α2), VD (β2) receptors
- Portal v: α-receptors = VC
- Adr/NA
- Hep a. biphasic VC → VD
- Portal v. → VD
- Glucagon → hepatic a. VD
- AII → VC hep a. & portal v.
- VASOPRESSIN = ↑R Hep A + ↓R Portal V.
- ∴ efficacious to Rx portal HTN
Explain the changes to drug metabolism when liver blood flow decreases (40 marks)
- Clearance of drug by liver depends on:
- HEPATIC BLOOD FLOW
- PLASMA PROTEIN BINDING
- HEPATIC ENZYME ACTIVITY
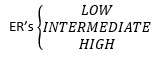
HEPATIC DRUG CLEARANCE = HBF x ER
- HEPATIC EXTRACTION RATIO = the fraction of drug entering liver in blood which is irreversibly removed (excreted) during one part of the blood through the liver
- HER is determined by free (unbound) drug fraction & by intrinsic clearance rates
- PPB → hepatocytes can only metabolise free drug ∴↓PPB = ↑HER
Intrinsic clearance (hepatic enzyme activity) = ability of liver to remove (metabolise) the drug in absence of restrictions imposed by drug delivery (i.e. HBF/PPB)
High Intrinsic Clearance
- Hepatocytes can only metabolise what they’re given
- Drug with high intrinsic clearance if affected by ∆HBF
- Hepatic metabolism is directly proportional to HBF
- ↓HBF = ↓↓drug metabolism
Low Intrinsic Clearance
- HBF will have minimal effect on drug metabolism
- ∆HBF produce inversely proportional ∆ER for drugs with LER ∴hepatic clearance is not depending on BF, but extremely dependent on intrinsic clearance
By clarifying drugs as:
- We can predict how intrinsic clearance & HBF will affect drug metabolism
- High ER = v. affected by HBF
- ↓HBF = ↓↓drug metabolism
- Low ER = not affected by liver BF very dependent on intrinsic clearance
HIGH ER
GTN
Lignocaine
PPF
Morphine
LOW ER
Diazepam
Warfarin
Phenytoin
Rocuronium
- Author: Krisoula Zahariou