I1i / 17B04: Describe how interstitial fluid recirculates to the vascular system
17B04: Exam Report
Describe how interstitial fluid recirculates to the vascular system.
10% of candidates passed this question.
Candidates had a limited understanding of this area of the syllabus. It was expected that answers would describe important concepts including the anatomy of venous structures, valves and lymphatics, permeability and factors which influence permeability. A description of hydrostatic forces, other pressures involved, and the role of osmotic and electric forces were
required.
I1i / 17B04: Describe how interstitial fluid recirculates to the vascular system
Definition
- Interstitial fluid is the fluid in the spaces between cells
- Component of ECF
- 16% of total body weight
Fluid Filtration Across Capillaries
- Fluid in the interstitium is derived by filtration and diffusion from capillaries
- Fluid filtration across capillaries is determined by
- Hydrostatic Pressures
- Osmotic Pressures
- Capillary Filtration Coefficient
- Hydrostatic & oncotic pressures described by ∆ Starling Forces:
NET FILTRATION PRESSURE = Kf (PC – Pi) – s (πC – πi)
Kf = Filtration Coefficient
- SA capillary walls x perm to H2O
- e. a ‘leaky’ capillary due to histamine will have high Kf
σ = Reflection Coefficient
- = Capillary permeability to proteins
- This value ranges from 0 – 1
- i.e. Hepatic sinusoids v. perm ~1
- CSF & glomerular v. low closer to 0
Pc = Capillary Hydrostatic Pressure
- Pushes fluid into interstitial space
- Determined by arterial P, pre-cap & post-cap sphincter resistance
Pi= Interstitial Fluid Hydrostatic Pressure
- Pushes fluid into capillary
ΠC = Capillary Oncotic Pressure
- Generated by plasma albumin
- Generates an osmotic force
- Which prevents fluid moving out of capillary
- Stable at 28mmHg through vessel length
Πi = Interstitial Fluid Oncotic Pressure
- Generated by protein concentration of interstitial fluid
- Promotes fluid movement out of capillary
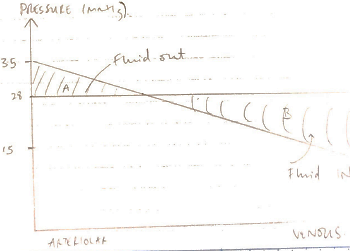
NFP is different at arterial & venous ends of caps
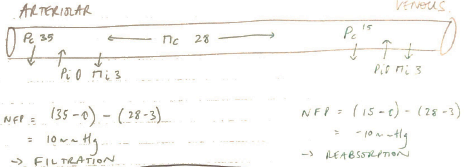
The fall in CAPILLARY HYDROSTATIC PRESSURE as blood flows from ARTERIAL à VENOUS end is responsible for the altered NFP
Fluid Loss
- NET FLUID LOSS from filtration is 4L/day
- This is all reabsorbed by lymphatics
Role of Lymphatic Circulation
Lymph = fluid which has entered lymphatic vessels from interstitial spaces
Anatomy
- Lymphatic capillaries = everywhere EXCEPT CNS, bone & cartilage
- Lymph vessels are blind-ending
- Made of endothelial cells with a highly permeable BM
- Possess flap valves between endothelial cells → permit one way entry of ISF
- Lymph caps drain into larger lymph vessels
- All lymph passes through LNs
- Lymph returns to circulation via:
- THORACIC DUCT → junction of L) subclavian & LIJ
- R) LYMPHATIC DUCT → junction of R) subclavian & RIJ
Return of Fluid
- Starling’s Forces result in:
- Net Filtration ~20mL/min at arterial end
- Net reabsorption ~18mL/min
- ∴2mL/min escapes into interstitium
- This fluid is returned to circulation by lymph at a rate of 2mL/min (at rest)
Lymph Flow
- Lymph flow 2mL/min (to return fluid from ISF)
- EXTRINSIC & INTRINSIC factors promote this
- Extrinsic: tissue pressure, skeletal m. activity, arterial pulsations → all compress lymph vessels
- Intrinsic: smooth m. wall contraction in large lymph vessels & presence of 1-way-valves → ensure unidirectional flow
- ↑flow with exercise
- If ISF volume > lymph drainage → OEDEMA
Interstitial Fluid Accumulation
Due to:
1. Imbalanced Starling Forces
- ↑PCg. fluid overload
- ↓πCg. malnutrition → ↓protein synthesis
- ↓Pig. negative pressure pulmonary oedema
- ↑πig. burns → plasma leak
2. Impaired Lymph Drainage
- Lymphoedema due to LN clearance or blockage i.e. infection
3. Kf ↑ / ↑ σ
- ↑Kf with infection/inflammation = leaky caps
- ↑s in tissues with higher protein permeability i.e. liver
- Author: Krisoula Zahariou