H1v / 18B09: Describe the renal handling of water
18B09: Exam Report
Describe the renal handling of water including the modulation of water excretion.
37% of candidates passed this question.
This question required a brief introduction of the role the kidney plays in water balance; a more detailed description of how water is handled as it passes through the various segments of the nephron (glomerulus, PCT, Loop of Henle, DCT and Collecting Duct); the modulation of water excretion by the kidney due to ADH (vasopressin) and how this operates; and the stimuli (osmotic and non-osmotic) for ADH secretion. Although worth mentioning in the context of the effect they have on water movement through the kidney, detailed explanations of Starling’s forces in the glomerulus, and of the operation and maintenance of the counter-current mechanism, were not required. More important was describing the control of water reabsorption in the collecting ducts (and thus modulation of water excretion by the kidney) under the influence of ADH.
H1v / 18B09: Describe the renal handling of water including modulation of water excretion
- Total body water (60% of weight = 42L in a 70kg M) is regulated by FEEDBACK MECHANISM
SENSORS (volume & osmolarity receptors)
↓
CENTRAL PROCESSOR (hypothalamus)
↓
EFFECTORS (kidneys, thirst centre)
- TBW = 42L
- GFR = 180L
- Water input must match output
- Obligatory urine loss = 600mOsm/day (urea, sulphates, metabolic byproducts)
- Makes minimum urine loss 430mL/day (1400mOsm/kg H2O)
But there is no ‘water receptor’ → water is regulated in order to:
- Maintain volume
- Maintain osmolality for the health of cells
∴ regulation of H2O is by volume & osmolality receptors
2 components of kidneys to H2O balance:
- PROX NEPHRON
- Reabsorbs H2O with sodium
- Isotonic
- Regulates ECF
- DISTAL NEPHRON
- Reabsorbs H2O independent of Na+
- Determined by ADH
- Maintains osmolality
H2O is absorbed by OSMOSIS → either directly through PM or through aquaporin channels
PCT
- Na+ is 50% of ultrafiltrate
- 65% Na+ is reabsorbed at PCT
- 65% H2O follows
- Maintains ISOOSMOTIC volume reabsorption
Desc. LOH
- Permeable to H2O, impermeable to solutes
- Na/K/2Cl reabsorption in Thick Asc Limb has set up a hyperosmolar medullary ISF
- ∴when isotonic tubule fluid arrives to Desc LoH, H2O reabsorption is driven into Medullary ISF (despite Na+ being impermeable here)
Thick Asc. LOH
- Impermeable to H2O, permeable to solutes
- Fluid entering Asc. limb is hypertonic due to Desc. limb H2O reabsorption without solute
- This drives thick asc. limb to reabsorb solutes via Na/K/2Cl transporter → leaving behind hypotonic tubule fluid
DCT
- Also impermeable to H2O, permeable to solutes
- Further solute reabsorption → further hyperosmolar tubule fluid
Collecting Duct: $$$
- H2O permeability of Collecting Duct is under physiological control → determines if urine is going to be hyper/hypo osmolar
- Depends on presence/absence of ADH
ADH
- Peptide hormone
- Produced by hypothalamic neurons
- Cell bodies in supraoptic & paraventricular nuclei
- Axons terminate in PPG
- ADH released from PPG → into blood
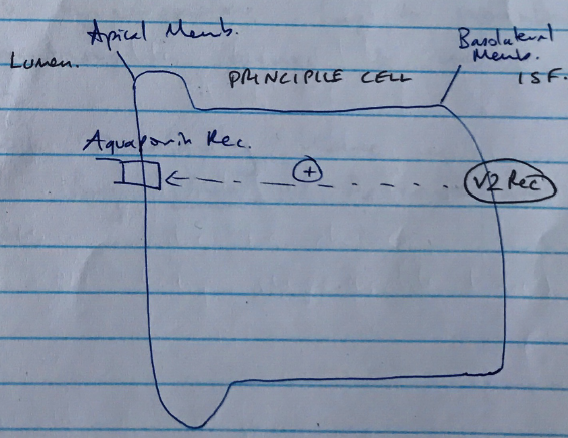
- @ PRINCIPLE CELLS of collecting duct
- V2 receptors (GPCR)
- ADH binding ↑cAMP
- Causes Aquaporin channel insertion on Apical membrane
- H2O reabsorbed by osmosis
No ADH
- Low H2O permeability
- Hypo-osmolar fluid entering collecting duct remains hypo-osmolar
- Na+ reabsorption continues without any H2O reabsorption
- Result → large volumes of hypo-osmolar (30mOsm/L) urine → KA WATER DIURESIS
NB: This is what happens pathologically in D.I where there is no ADH production & massively dilute urine up to 25L/day produced!
High ADH
- High H2O permeability of Cortical & medullary collecting duct
- Cortical: hypo-osmotic fluid undergoes rapid osmosis via aquaporins to restore tubule fluid to be isosmotic (300mOsm/L)
- Medullary: even greater H2O reabsorption of cortex CD because medulla ISF has potential to become v. hyper-osmolar (up to 1400mOsm/L)
- ∴H2O reabsorption occurs to restore isotonicity
- The high osmolarity here is generated by urea & the counter-current multiplier
Control of ADH Secretion
Baroreceptor Control of ADH
- ↓ECF (i.e. diarrhoea, vomiting)
- ↓BaroR firing
- ↑ADH secretion
- ↑H2O reabsorption at CD
+ very high ADH levels = mass VC by ADH (vasopressin)
- arteriole VC → ↓GFR → ↓Na/H2O loss → restores volume
Osmoreceptor Control of ADH
- To restore osmolality you need to +/- H2O without ∆ Na+
- ∴when osmoreceptors are stimulated, this is what results of their ADH secretion:
- OSMORECEPTORS
- Surround 3rd ventricle
- Capillaries with +++ fenestration
- Allows their interstitium to ∆ with plasma composition rapidly
- Osmoreceptors send info to Hypothalamic cells
- Secrete ADH
- ↑free H2O → ↓ADH secretion → CD H2O permeability ↓with dehydration → ↑ADH secretion → ↑aquaporins → ↑H2O reabsorption
- Dehydration → ↑ADH secretion → ↑aquaporins → ↑H2O reabsorption
NB: SIADH = large inappropriate ADH secretion → mass H2O reabsorption
- Author: Krisoula Zahariou