F10ii / 18B14 : Explain the detection and response to hypoxaemia
18B14: Exam Report
Explain the detection and response to hypoxaemia.
34% of candidates passed this question.
A logical approach to answering this question included a definition of hypoxaemia and then a discussion of the sensors, integrators and effectors involved. It was expected that candidates would cover the peripheral chemoreceptor response (including the respiratory, cardiovascular and autonomic effects), time course of the ventilatory response, hypoxia-inducible factors, vascular effects (hypoxic vasoconstriction in the pulmonary circulation and vasodilatation in the systemic circulation) and metabolic changes (switch to anaerobic metabolism). No marks were awarded for discussing the causes of hypoxaemia. Many candidates incorrectly stated that hypoxaemia is detected by the central chemoreceptors.
F10ii / 18B14: Explain the detection and response to hypoxaemia
Definition
A reduction of oxygen partial pressure in the blood (<60mmHg)
Detection
- Peripheral ChemoR monitor ↓PaO2, ↑PaCO2, ↓pH
- Bilateral CAROTID BODIES near bifurcation of Common Carotid A.
- Have large sinusoid
- Very high rate of perfusion, x 10 their own metabolic requirement
- Their arterial/venous pO2 difference is v.small
- ∴detect & rapidly (1 – 3 secs) respond to ∆PaO2
NB: Stimulation by ↓pO2 not oxygen content ∴not stimulated by AN, CoHb, MetHb
Response
- Glomus Type 1 cell
- Hypoxaemia with ↓intracellular ATP
- ↑Ca2+ intracellularly, released by mitochondria
- ↑firing of T1 glomus cells
- Make synaptic contact with Glossopharyngeal n. (IX)
- Stimulates hypoxic drive for ventilation at pO2 < 80mmHg
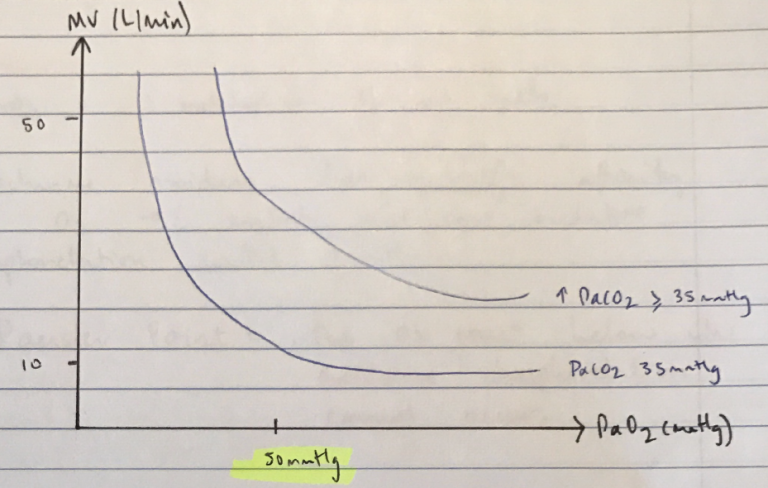
- Steep ↑MV at PaO2 < 50mmHg
Neurological
- ↑MV = steep @ <50mmHg
- Cerebral hypoxia = lactic acidosis = ↓pH = further ↑MV
Circulatory
- Mass VD (except pulm. vessels) → due to ↑[adenosine] generated by hypoxia
- Hypoxia will ↑BF to all tissues, especially brain
- Hypoxia VD will overcome cerebral VC due to hypocapnia = ↑↑↑CBF
- Cerebral hypoxia = mass symp. outflow
- Hypoxic pulm. VC = ↑PA pressures
- R) shift ODC due to ↑2, 3 DPG & acidosis
Metabolism
- ↓PaO2 = ↓metabolism of all cells
- Cytochrome oxidase has high affinity for O2 → ∴mitochondria will continue oxidative phosphorylation until 1mmHg
Pauster Point = the O2 concentration below which oxidative phosphorylation cannot occur
- Author: Krisoula Zahariou