H1i / 19A04 / 17A18: Outline the functional anatomy of the kidneys + regulation of renal blood flow
19A04: Exam Report
Outline the functional anatomy of the kidney (40% of marks). Outline the regulation of renal blood flow (60% of marks).
71% of candidates passed this question.
It was expected that answers include sections on the blood supply, the nephron (including the difference between the cortical and juxta-medullary nephrons) and innervation. A number of candidates failed to quantify renal blood flow and to define autoregulation. The concept that it’s the flow that’s regulated was not described by some. Tubuloglomerular feedback was generally described correctly but a reasonable number had the blood flow increasing when an increased sodium was sensed at the macula densa.
17A18: Exam Report
Outline the functional anatomy of the kidneys (40% of marks). Outline the regulation of renal blood flow (60% of marks).
67% of candidates passed this question.
Candidates who scored well weighted their answers according to the marks allocation outlined in the question and adopted a good structure. A number of andidates confused the roles of tubuloglomerular feedback and the renin angiotensin aldosterone pathway.
H1i / 19A04 / 17A18: Outline the functional anatomy of the kidneys (40 marks) & Outline the regulation of renal blood flow (60 marks)
- The functional unit of the kidney is the NEPHRON
- The nephron is made up of the renal tubule & the renal corpuscle
- Each kidney has ~1 million nephrons
- A nephron is a hollow tube made of a single cell layer & consists of:
- Renal Corpuscle
- Proximal Tubule
- Loop of Henle
- Collecting duct system
- Each part of the nephron is made of cells specific to the function of that portion of the nephron → hence, we can describe the functional anatomy
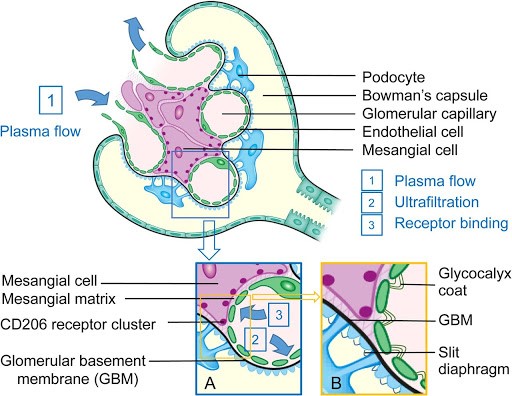
Renal Corpuscle
- ULTRAFILTRATE = passive movement of protein free fluid from glomerular capillaries to Bowman’s capsule
- Corpuscle is made up of GLOMERULAR CAPILLARIES invaginated by the BOWMAN’S CAPSULE, which is a blind end of the renal tubule
- Glomerulus is a capillary network supplied by the AFFERENT CAPILLARY & drained by the EFFERENT CAPILLARY
- Fluid passes from Glom Caps → Bowman’s Space by the action of opposing HYDROSTATIC & ONCOTIC PRESSURES
- The filtration barrier of the RENAL CORPUSCLE is formed by 3 layers:
- Capillary Endothelium
- BM
- Bowman’s Corpuscle Epithelium
Capillary Endothelium
- Fenestrated → i.e. contains holes
- Freely permeable to H2O, small solutes, most proteins
- NOT permeable RBC, WBC, platelets
- Have negatively charged glycoproteins, ∴retards filtration of large anionic proteins
- Also! synthesise vasoactive substances → NO (→ VD), ET-1 (→ VC)
Basement Membrane
- Covers the endothelial cells
- Made of negatively charged proteins
- Mainly filters based on charge
Proximal Tubule
- Collects a large volume of ultrafiltrate from the Bowman’s Capsule
- Reabsorbs 60% back into the bloodstream
- Proximal tubule cells have an extensive APICAL MEMBRANE with a BRUSH BORDER
- The BASOLATERAL MEMBRANE is highly invaginated with many mitochondria
- REABSORBS: H2O, Na, Cl, K, HCO3, Ca2+, glucose, urea, phosphate, any filtered proteins
- SECRETES FROM BLOOD: H+, NH4+ (ammonium), urate, organic ions + cations
Loops of Henle
- Thin limbs have basic apical & basolat. membrane
- LoH creates an ↑interstitial osmotic gradient in medulla to allow reabsorption of H2O from collecting ducts & production of concentrated urine (1400mOsm/kg) with ADH
- Desc. Limb → reabsorbs H2O
- Thick Asc. Limb → reabsorbs Na, K, Cl, HCO3 & secretes H+
- Thick Asc. Limb cells have many mitochondria & extensive folding of BASOLAT MEMBRANE
Collecting Duct → 2 cell types
Principle Cells
- NaCl reabsorption
- K+ secretion
- Stimulated by aldosterone
Intercalated Cells
- Acid-base balance
*** NOTE: All cells in the nephron except intercalated cells have SINGLE NON-MOTILE CILIA
- Mechanosensors: ∆ flow rate
- Chemosensors
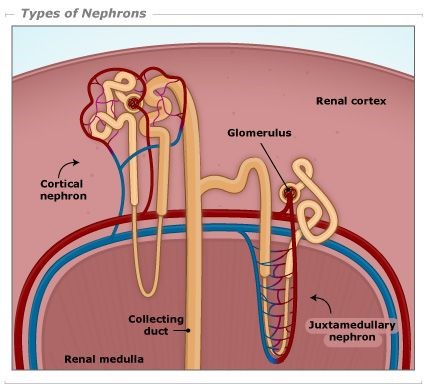
Superficial & Deep Nephrons
- Position of corpuscle in cortex determines length of LoH
- Superficial cortical nephrons → short LoH
- Juxtamedullary (deep) nephrons have their corpuscle close to medulla
- They have long loops
- Their efferent arteriole forms the PERITUBULAR CAPS & also the VASA RECTA
- Peritubular caps = caps around PCT & DCT that function in reabsorption
- Vasa recta = caps enveloping LoH that function to maintain [ ] gradient
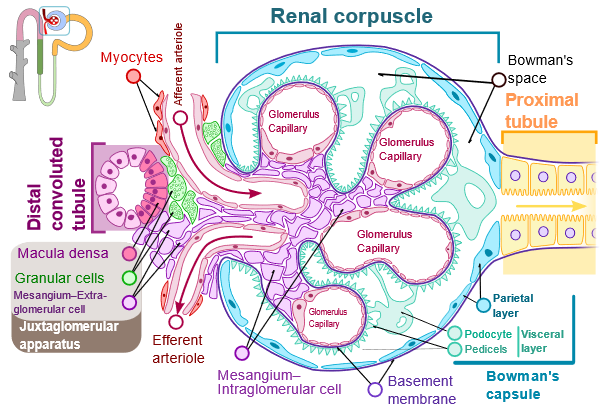
Juxtaglomerular Apparatus
- One component of the TUBULOGLOMERULAR FEEDBACK
- Juxtaglomerular app. is made of 3 structures:
- Macula densa
- Extraglomerular mesangial cells
- Granular cells
- Juxtaglom app. represent distinct part of nephron where Thick Asc. LoH passes through aff. & eff. arteriole
Granular Cells
- Of Aff. arteriole
- Make & store RENIN
Macula Densa
- Of Thick Asc. Limb
- In contact with Mesangial cells & Granular cells
- Sense passing fluid flow rate
- Produce a local VC substance
Anatomy
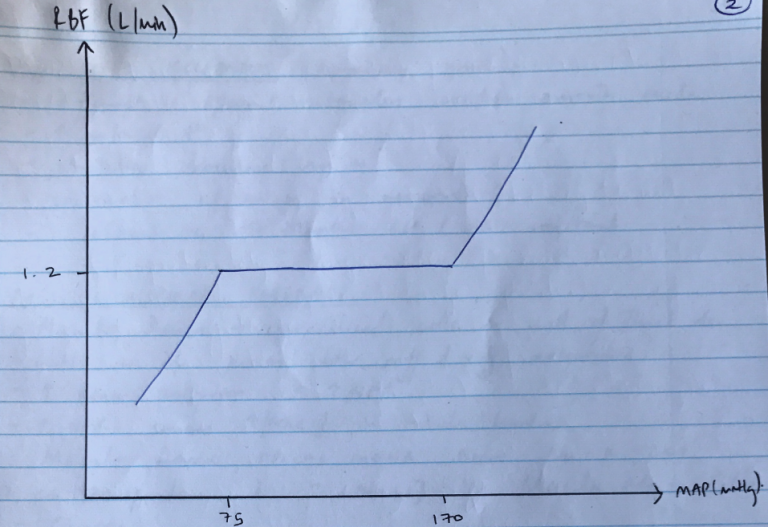
- RBF = 20% CO
= 1.2L / min
= 600mL / kidney / minute
- RBF is not evenly distributed
- 90% → cortex
→ flow-dependent function
→ glomerular filtration & reabsorption
→ 5 mL / g / min
→ PaO2 = 50mmHg
- 10% → medulla
→ outer medulla = 1 mL / g / min
→ inner medulla = 0.2 mL / g/ min
→ Urine concentration
→ PaO2 = 8 – 15mmHg
Therefore, even though medulla is more metabolically active (& extremely vulnerable to hypoxic injury), majority of BF to cortex is to drive filtration of plasma & provide adequate GFR.
RBF Regulation
- Q = blood flow
- ∆P = MAP – venous pressure for that organ
- R = resistance to flow through that organ
- GFR is strongly influenced by renal perfusion pressures
- Because of the many activities which can change arterial pressure, the kidneys autoregulate their BF to ensure a constant RBF → & ∴constant GFR over a wide range of pressures
- This is KA AUTOREGULATION = the intrinsic ability of an organ to maintain a constant blood flow despite changes in perfusion pressure
- Between MAP 75 – 170mmHg, RBF remains constant
- GFR remains constant 125mL/min between these pressure as well
R = ∆P/R
- ∴when ∆P, autoregulation is achieved by changing R (vascular resistance)
- Main resistance vessels of kidney are afferent & efferent arterioles
- 2 mechanisms:
- MYOGENIC → responds to ∆ arterial P
- TUBULOGLOMERULAR FEEDBACK → respond to ∆[NaCl] of tubule fluid
1) Myogenic Mechanism
- Especially quick!
- Afferent & efferent arterioles contain smooth m.
- ↑arterial P
- Stretches vascular smooth m.
- Contraction of smooth m. in response
- ∴afferent VC → maintain RBF & GFR constant
2) Tubuloglomerular Feedback
- Macula Densa → specialised cells in wall of Thick Asc. LoH as it passes b/w afferent & efferent arterioles
- ↑renal perfusion = ↑GFR
- ↑GFR causes ↑[NaCl] in tubule lumen
- Macula densa APICAL MEMBRANE have Na-K-2Cl co-transporter
- ↑[NaCl] in Macula Densa Cells
- Causes:
- ↑ATP release in BLM of macula densa cells
- ↑adenosine production
- Adenosine binds A1 receptors of afferent smooth muscle cells → VC → restores GFR
- NB: Macula Densa produce NO if ↓GFR to restore GFR
- Author: Krisoula Zahariou