H1ii / 19B02: Renal blood flow
19B02: Exam Report
Describe renal blood flow and its regulation (80% of marks). Outline the impact of adrenoreceptor agonists on renal blood flow (20% of marks).
64% of candidates passed this question.
This question was well answered by most candidates. The description of renal flow involves a brief comment of the anatomy including interlobar, arcuate, interlobular arteries, then afferent and efferent arterioles – 2 sets of capillaries and then corresponding veins and better answers made the distinction better cortical and medullary flow and went on to detail the consequence of this. Renal blood flow is autoregulated and most candidates describe well the various mechanisms
around myogenic and tubuloglomerular feedback. Additional marks were gained with by discussing renal vascular resistance and how this may be varied. The impact of adrenoreceptor agonists is varied but generally sympathomimetic agents will vasoconstrict and therefore increase renovascular resistance and result in a decrease renal blood flow. The relative impact on afferent vs efferent arteriolar tone may alter glomerular perfusion pressure.
H1ii / 19B02: Describe renal blood flow and its regulation (80 marks). Outline the impact of adrenoreceptor agonists on renal blood flow (20 marks).
Anatomy
- RBF = 20% CO
= 1.2L / min
= 600mL / kidney / minute
- RBF is not evenly distributed
- 90% → cortex
→ flow-dependent function
→ glomerular filtration & reabsorption
→ 5 mL / g / min
→ PaO2 = 50mmHg
- 10% → medulla
→ outer medulla = 1 mL / g / min
→ inner medulla = 0.2 mL / g/ min
→ Urine concentration
→ PaO2 = 8 – 15mmHg
Therefore, even though medulla is more metabolically active (& extremely vulnerable to hypoxic injury), majority of BF to cortex is to drive filtration of plasma & provide adequate GFR.
RBF Regulation
- Q = blood flow
- ∆P = MAP – venous pressure for that organ
- R = resistance to flow through that organ
- GFR is strongly influenced by renal perfusion pressures
- Because of the many activities which can change arterial pressure, the kidneys autoregulate their BF to ensure a constant RBF → & ∴constant GFR over a wide range of pressures
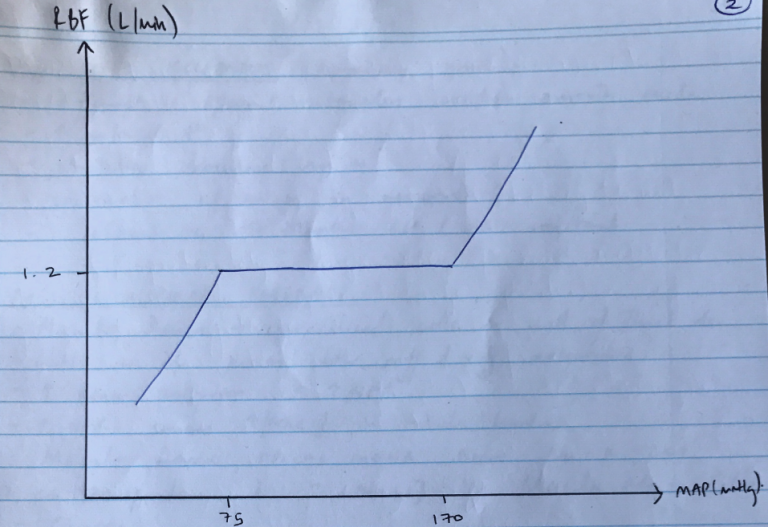
- This is KA AUTOREGULATION = the intrinsic ability of an organ to maintain a constant blood flow despite changes in perfusion pressure
- Between MAP 75 – 170mmHg, RBF remains constant
- GFR remains constant 125mL/min between these pressure as well
R = ∆P/R
- ∴when ∆P, autoregulation is achieved by changing R (vascular resistance)
- Main resistance vessels of kidney are afferent & efferent arterioles
- 2 mechanisms:
- MYOGENIC → responds to ∆ arterial P
- TUBULOGLOMERULAR FEEDBACK → respond to ∆[NaCl] of tubule fluid
1) Myogenic Mechanism
- Especially quick!
- Afferent & efferent arterioles contain smooth m.
- ↑arterial P
- Stretches vascular smooth m.
- Contraction of smooth m. in response
- ∴afferent VC → maintain RBF & GFR constant
2) Tubuloglomerular Feedback
- Macula Densa → specialised cells in wall of Thick Asc. LoH as it passes b/w afferent & efferent arterioles
- ↑renal perfusion = ↑GFR
- ↑GFR causes ↑[NaCl] in tubule lumen
- Macula densa APICAL MEMBRANE have Na-K-2Cl co-transporter
- ↑[NaCl] in Macula Densa Cells
- Causes:
- ↑ATP release in BLM of macula densa cells
- ↑adenosine production
- Adenosine binds A1 receptors of afferent smooth muscle cells → VC → restores GFR
- NB: Macula Densa produce NO if ↓GFR to restore GFR
Sympathetic Nerves
- & eff. Arterioles innervated by symp n’s
- Basal sympathetic tone is minimal
- ↑ECF V → symp n. release Na & adrenaline → α1 receptor of aff arterioles → ↓RBF & GFR
Adrenoreceptor
a
Agonist
Phenylephrine
Effect on RBF
↓
Adrenoreceptor
a
Agonist
Metaraminol
Effect on RBF
↓
Adrenoreceptor
a/β
Agonist
Adrenaline
Effect on RBF
↓
Adrenoreceptor
a/ β
Agonist
Noradrenaline
Effect on RBF
↓
Adrenoreceptor
a/β
Agonist
Ephedrine
Effect on RBF
↓
Adrenoreceptor
β
Agonist
Isoprenaline
Effect on RBF
↑
Adrenoreceptor
β
Agonist
Dopamine
Dopamine (low dose) dilates renal arterioles via Dopaminergic Receptors
Effect on RBF
↑
Hormones
Vasoconstrictors
A II
Renin
Endothelin
Adenosine
Vasodilators
Prostaglandins
NO
ANP/BNP
Bradykinin
A II
- Produced systemically & locally
- Constricts aff & eff
- ↓RBF & GFR
Endothelin
- Secreted by renal endothelial cells in response to AII, shear stress
- Profound VC aff & eff. Arterioles
- ↓RBF & GFR
Adenosine
- VC of aff. arteriole
- Role of TUBULOGLOMERULAR FEEDBACK
Prostaglandins
- Produced in pathological conditions e.g. haemorrhage
- ↑RBF without ∆ GFR
- Also dampens effects of symp. n & AII which is important to protect against renal ischaemia
NO
- Produced by endothelium
- Many stimulants: shear forces, ACh, histamine, BK, ATP
- VD aff. & eff. Arterioles
ANP/BNP
- Secreted by cardiac atria when ↑ECFV
- VC aff. & eff. Arterioles = ↑GFR with little ∆RBF
A note on pressure diuresis…
- Deep (juxtamedullary) nephrons are not autoregulated
- ∴when BP ↑, blood is diverted from cortical to juxtamedullary nephrons & vasa recta capillaries
- This washes away solutes from medulla (Na, Cl, Urea0 & ↓urinary concentrating ability
- This loss of H2O and solutes KA PRESSURE DIURESIS
- Author: Krisoula Zahariou