H1iv / 20A04 / 15B22: Countercurrent
20A04: Exam Report
Explain the counter-current mechanism in the kidney.
63% of candidates passed this question.
Higher scoring candidates described the counter-current multiplier mechanism, the counter- current exchanger and the contribution of urea cycling to the medullary osmotic gradient. Detailing the mechanisms as to how they may be established, maintained and or regulated. Descriptions of the multiplier (LOH) alone did not constitute a passing score. Values for osmolality at the cortex & medulla and within the different parts of the LOH was required. A description of the counter-
current exchanger system where inflow runs parallel to, counter to and in close proximity to the outflow was expected. This could have been achieved by describing the anatomical layout of the loop of Henle and the vasa recta.
15B22: Exam Report
Describe the counter-current mechanisms in the kidney (60% of marks) and in the skin (40% of marks).
48% of candidates passed this question.
Most answers gave a good account of counter currents in the kidney but few described the generation of the counter current multiplier arrangement. Many candidates did not discuss counter current mechanisms in the skin but instead, focussed on thermal control by the skin.
H1iv / 20A04 / 15B22: Explain the counter-current mechanism in the kidney. Describe the counter-current mechanisms in the kidney (60 marks) + the skin (40 marks)
- Counter-current = a mechanism of physiology, whereby there is cross-over of property between two flowing bodies, flowing in opposite direction to each other
- In humans:
- KIDNEYS → exchange of H2O
- SKIN → exchange of heat
- Function: to allow maximum property transfer than would be possible with a parallel system because it creates a bigger gradient for property exchange
Skin
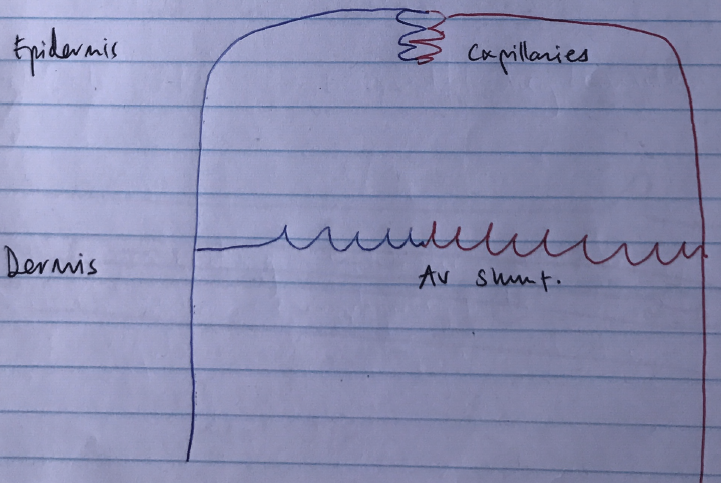
- There are 2 networks of blood in the skin:
- CAPILLARIES → provide nutrients, controlled by O2 & metabolic by-products
- AV SHUNTS → aid thermoregulation, respond to Na/ACh
- So ↑temp → AV shunt VC → blood diverted to caps in epidermis → heat loss by radiation
Counter Current of Skin
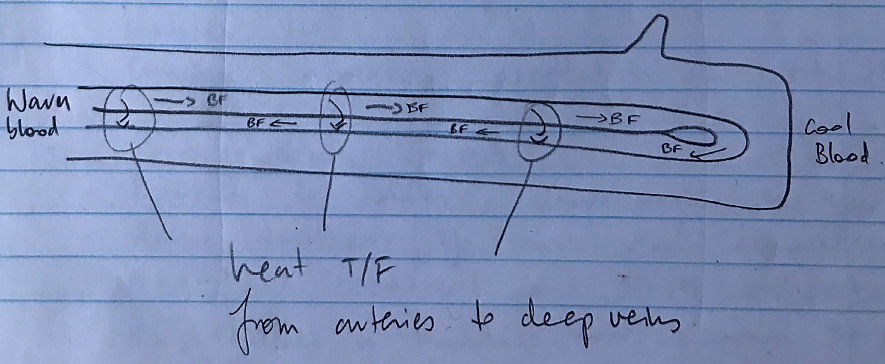
- In cold weather there is ↓BF to extremities
- Counter current heat exchange b/w arteries & deep veins short circuits heat loss by radiation from the skin
- For example:
- Arterial blood delivers warm blood
- Deep veins wrapped around arteries
- Counter-current flow allows heat t/f from arteries → deep veins
- Heat is returned to trunk
- Hand is cooled without heat loss
Kidneys
Counter Current of Kidneys
- 2 counter current mechanisms in kidney:
- COUNTERCURRENT MULTIPLIER → makes hyperosmolar tubule fluid
- COUNTERCURRENT EXCHANGER → ensures hyperosmolar gradient is not lost
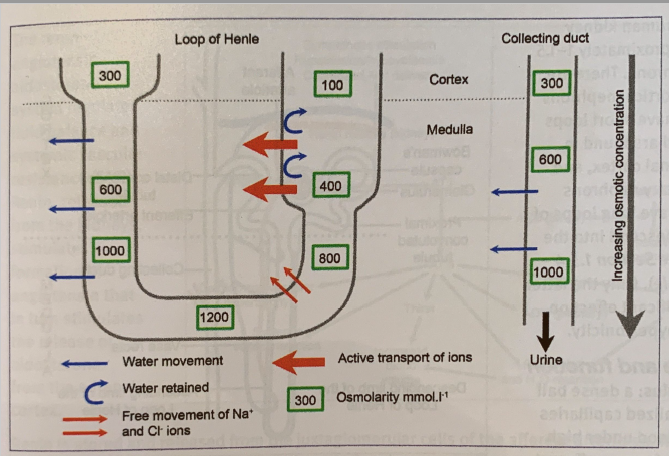
Counter-Current Multiplier:
- Occurs in juxtamedullary nephrons
- It is the development of osmotic gradients by LoH which allows the formation of concentrated urine
- Only possible because LoH has different permeabilities along its length
- Thin Ascending Limb
- Permeable to solutes, impermeable to H2O
- Passive movement of solutes out of tubules
- Increases osmolality of medulla ISF
- Thin Descending Limb
- Permeable to H2O, impermeable to solutes
- H2O moves down [ ] gradient into medulla ISF
- Causing increasing osmolality of tubule fluid
- Thick Ascending Limb
- Permeable to solutes, impermeable to H2O
- Active transport of ions via luminal (urine) Na/K/2Cl cotransport and Na/H antiporter
- Na/K/aTPase on basolateral (blood) maintain the gradient
- Dilutes tubule fluid, increases osmolality of medulla iSF
- NET RESULT → osmolality of ISF & tubule fluid in desc LoH ↑whilst osmolality of tubule fluid in Asc LoH ↓
- Thin Ascending Limb
- The counter-current flow of tubule fluid in LoH allows multiplication of medullary ISF osmolality
- The process repeats & repeats itself along the tubule length, so the longer the hairpin, the more the medulla ISF can become hyperosmolar
- Fluid entering LoH is 300mOsm/L → can be concentrated up to 1400mOsm/L at tip of LoH
Countercurrent Exchanger:
- Vasa recta derive from efferent arterioles of juxtamedullary nephrons
- Arranged as loops along LoH
- If these vessels were to absorb all solutes of ISF, the [ ] gradient would be eliminated
- It is an exchanger → ∴ no E necessary
- Desc & asc. VR exchange solutes and the Asc. VR removes H2O
NaCl
↓
Leaves thick asc. LoH
↓
Accumulates in medulla ISF
↓
Absorbed by desc. VR
↓
Travels in in vessel lumen to asc. VR
↓
Returns to medulla ISF
H2O
↓
Travels through desc. VR
↓
Enters medulla ISF
↓
Oncotic P canoes it to diffuse into asc. VR
↓
Continues into circulation
→ This whole process is facilitated by the slow BF through the VR (because if it was fast it wouldn’t allow enough time for solute exchange). The slow BF is due to the anatomy of the hairpin
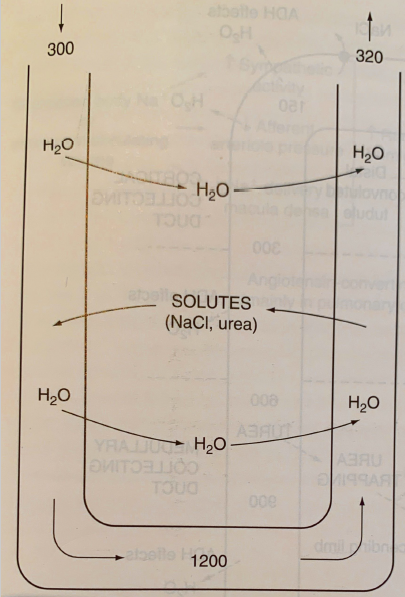
Further Concentration by ADH
- ADH helps concentrate urine further
- ↑permeability of collecting duct (all regions) to H2O
- Principle Cells
- V2 receptors on Basolateral (blood) membrane activates AC
- ↑cAMP (2nd messenger)
- Aquaporin channels insert onto luminal (urine) membrane
- ↑↑↑↑H2O permeability
- Activates UREA TRANSPORTERS → absorbs even more H2O following urea
- ADH ↑Na/K/2Cl activity to Thick Asc. → ∴concentrating urine further
- ↑permeability of collecting duct (all regions) to H2O
Urea Recycling
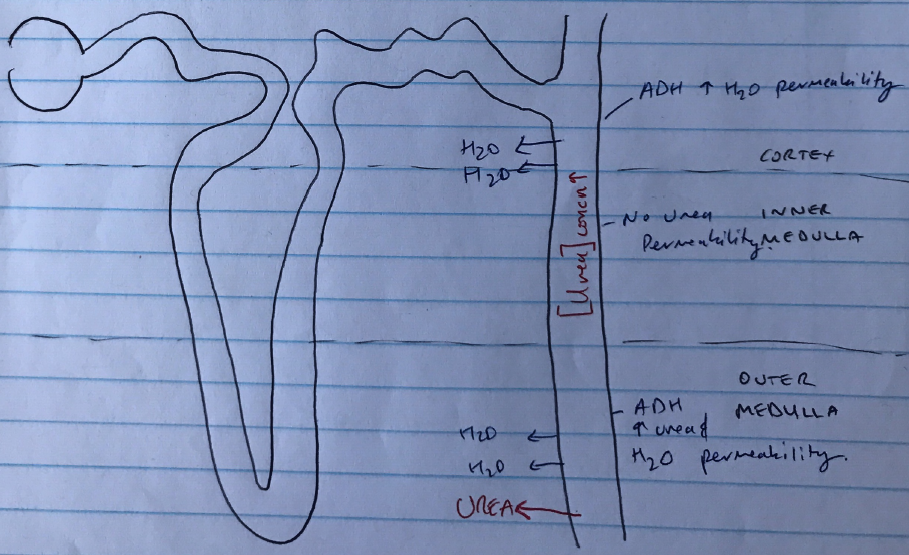
- LoH, DCT, cortex collecting duct are all impermeable to urea
- ∴[urea] keeps building in tubule fluid & it is in very high [ ] in Medullary Collecting Duct
- Under influence of ADH → medullary collecting duct becomes permeable to urea → further concentrates medulla ISF osmolality
- In fact it is urea alone that results in half the concentrating ability of the kidneys!
- Author: Krisoula Zahariou