Pv / 20A08 / 15B06: Describe the production, metabolism and role of lactate
20A08: Exam Report
Describe the production, metabolism and role of lactate.
16% of candidates passed this question.
Better answers used the categorisation in the question as a structure for their answer. Many candidates gave a good description of lactate production from glycolysis, increasing with accumulation of NADH and pyruvate, when these are unable to enter Krebs cycle. There were however, many vague and incorrect descriptions as to what lactate is and its physiological role.
Many candidates suggested that its presence is abnormal or pathological. Most answers demonstrated a superficial understanding and physiological detail of lactate’s role as an energy currency in times of oxygen debt. Higher scoring candidates often mentioned non-hypoxic causes of pyruvate accumulation which include; circulating catecholamines, exercise, sepsis or lack or mitochondria (RBCs). Mention of the relative ATP production of the two fates of pyruvate was
also noted in more complete answers. The Cori cycle was generally superficially described. A key role of lactate is the ‘lactate sink’, allowing a period of ongoing ATP production from glycolysis when cells become oxygen deplete or the Kreb’s cycle is inhibited; few candidates detailed or highlighted this.
15B06: Exam Report
Describe the formation and the metabolic fate of lactate. Outline its role in energy production.
21% of candidates passed this question.
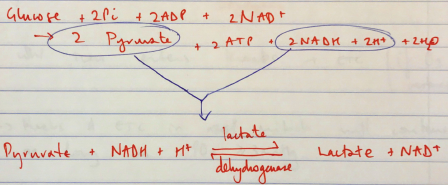
It was expected that the answer would include comments on lactate generation from glucose via pyruvate and the metabolic linkage of nicotinamide adenine dinucleotide (NAD). Lactate regenerates NAD+ (pyruvate is reduced to lactate while NADH is oxidized to NAD+ ). The citric acid cycle and the electron transport chain occur in the mitochondria of cells, and will only
proceed in the presence of oxygen.
One molecule of glucose produces 2 ATP anaerobically (pyruvate to lactate) vs 26 aerobically (pyruvate enters TCA cycle). Total production is about 1500 mmols/day with blood levels resting value of 1–1.5 mmol/L to a peak of 10–15 mmol/L.
Lactate can be used in 3 ways:
1. Conversion to glucose via gluconeogenesis in the liver and release back into circulation (Cori cycle). This is the fate of 80 % circulating lactate from tissues low in oxygen (e.g. exercising muscle with low pO2) or red blood cells (no mitochondria). The production from glucose in RBC’s is the Embden-Meyerhoff pathway.
2. Consumed as a fuel e.g. heart (20% of circulating lactate)
3. Mitochondria and oxygen
Oxidation back to pyruvate by well-oxygenated muscle cells, heart cells, and brain cells pyruvate is then directly used to fuel the Krebs cycle (generating 28 mmols ATP)
Lactate generation from muscle is increased with B1 mediated stimulation e.g. from adrenalin.
This topic is well covered in Power and Kam Principles of Physiology for the Anaesthetist, 3rd Edition, although some of the details are in several different sections.
Most candidates showed some understanding of the role of glucose in the production of pyruvate to lactate. However, the differential ATP production, the role of NADH availability and how oxygen and the role of mitochondria were involved was less well handled. Better answers described the normal generation of lactate in some tissues (e.g. RBC) and role of muscle and liver in metabolism back to glucose (Cori cycle) and the role of lactate as a metabolic substrate in some organs. Marks were awarded for normal production values and blood levels.
Pv / 20A08 / 15B06: Describe the production, metabolism and role of lactatev
Definitions
Lactate = a 3 carbon molecule with a carboxyl group at one end that can accept a hydrogen ion to form lactic acid
pKa = 3.9
Normal range < 2mmol/L
Production
- Cells need E for work
- E is generated from metabolic fuel
- Fuels are oxidised to release E
- Oxidation = removal of e– at high potential & transferring them to a lower potential ∴releasing E
- Removed e– must be transferred to an e– acceptor which is transportable, H2O soluble & generally available
- O2 is the e– acceptor used in cells
- But O2 is too reactive to be immediate oxidising agent → ∴intermediates NAD+ + FAD are e– carriers between metabolic pathways and O2 is used in the mitochondria
- NAD+ + FAD are reduced by Glycolysis & Krebs to NADH + H+ + FADH2 → these carry e– to ETC
- In the ETC the e– are transferred along a series of carriers with low potential until combining with O2 to form H2O
- This is how ATP is formed
- O2 is used @ end of ETC
- If O2 is N/A, NAD+ & FAD are converted to NADH + H+ & FADH2 by Law of Mass Action, the equation STOPS
- Anaerobic metabolism occurs when E demands exceed aerobic supply
- Anaerobic metabolism continues:
∴ Glycolysis can keep going
Lactic Acid Fate
- 20% → diffuses into blood & utilised by myocytes which are very good at converting lactate back to pyruvate for E
- 80% → metabolised for E
- Liver converts lactate to glucose (gluconeogenesis) & releases glucose back to circulation (CORI CYCLE)
- Travels to mitochondria: oxidised back to pyruvate
- Which then enters Krebs → ETC (if O2 supply restored)
- Krebs & ETC in mitochondria will continue as long as PO2 ≥3mmHg
- Glycolysis occurs in cytoplasm & doesn’t require O2
- Anaerobic = 2 ATP/glucose
- Aerobic = 38 ATP/glucose
∴Anaerobic much less efficient
- Each day body produces 150mmol of excess lactate
- Cycles internally ∴ normally no fixed net acid production
- This equation is happening ⮂ all the time
- Cells producing lactate: skin, brain, RBC (no mitochondria), Gut, skeletal m.
- ↑Production
- ↑skeletal m. activity (b1 stimulation)
- Pregnancy = placenta ↑lactate production
- Renal threshold 6mmol/L → ∴at normal levels no lactate is excreted in urine
- Small amount of filtered lactate (180mmol/day) is fully reabsorbed
- Author: Krisoula Zahariou