Q1i / 21A03 / 16A06: Platelets
21A03: Exam Report
Outline the formation, structure, and function of the platelet
79% of candidates passed this question.
This question was divided in three sections to help candidates formulate an answer template. The first section required a brief outline of the formation of platelets from pluripotent stem cells via megakaryocytes. The second section required an outline of platelet structure highlighting the special features such as, an absence of a nucleus, the presence of an external glycocalyx layer, specific surface receptors, contractile proteins, dense tubular system and granules. The third section was about platelet function where the expected focus was on the role of platelets in haemostasis. This required outlining the mechanism of platelet plug formation by adhesion-activation-aggregation, interactions with the coagulation cascade and role of platelets in clot contraction as well as fibroblast invasion. Although many candidates were able to answer the first section reasonably well, there was a noticeable knowledge deficit in the latter two sections. A significant proportion of answers had missing information on platelet structure and lack of structure in outlining platelet function.
16A06: Exam Report
Outline the formation, structure and function of the platelet.
50% of candidates passed this question.
The structure of the question outlined exactly what was expected. Platelets are formed in the bone marrow from budding of megakaryocytes. Granulocyte colony stimulating factor and thrombopoeiten play a role in the process and they have a life span of about 10 days. It was expected candidates could describe or draw the structure detailing they have no nucleus, the presence of mitochondria and granules and provide some detail of the important external surface proteins (glycoproteins, ABO, human platelet antigens). Better answers also described the internal microtubule structure and related this to function (allows contraction and shape change). The description of function required detail around the importance of platelet plug formation and the role of adhesion, aggregation and activation in this process.
Q1i / 21A03 / 16A06: Outline the formation, structure & function of the platelet
Version 1
Definition
A blood component involved in clot formation
Structure
- Small colourless disc
- 2 – 3µm (50% diameter RBC)
- Plasma [ ] 120 – 450 x 109
- Annucleated → cannot synthesise protein
- Ag’s
- HLA Class I, ABO, HPA 1 – 5
- Potential to cause transfusion reaction
- 4 zones: outer → inner
Peripheral Zone
- Many glycoproteins required for adhesion/activation/aggregation g. GP IIb/IIIa
Sol-Gel Zone
- Many microtubules & microfilaments
- Allow plats to maintain shape
Organelle Zone
- Rich in platelet granules
- α-granules = clotting mediators e. vWF, Factor V, VIII, fibrinogen, chemotactic agents
- δ granules = ADP, Ca2+, 5HT, all activating platelets
Membranous Zone
- Dense tubular system (actually the SER from Megakaryocytes)
- Synthesises Thromboxane A2 (TXA2)
↓
When released, activates & aggregates new platelets
Formation
Pluripotent Stem Cell → CFU → CFU-M → Megakaryocyte
- From MEGAKARYOCYTES (MK)
- Regulated by Thrombopoeitin (hormone of liver & kidneys) which bunds MK PM
- Divides without mitosis → MK enlarge & platelets bind off from PM
- Young platelets → mature in spleen
- Mature platelets last 10 days
- Degraded by RES cells of spleen/liver
Function
Form a platelet plug
Adhesion
- Intact endothelium prevents anticoagulation by NO, prostacyclin, CD39
- Endothelial cells are attached to collagen subendothelial layer by vWF (which is stored in platelets)
- When endothelial layer is disrupted → platelets anchor to exposed endothelium → bind to collagen
- Direct via GP Ia/IIa
- Via vWF to G Ib/IX
Activation
- Resting platelets inhibited by NO, Prostacyclin & a pump which pumps Ca2+ out
- Activation starts after adhesion
- Plat granule contents released by
- Collagen exposure
- Thrombin
- Granule secretion → ADP, 5HT, Ca2+
- ↑intrac Ca2+
- GP IIb, IIIa receptor activation
- ↑Thrombin
- ↑Thromboxane A2 → ↓cAMP → VC & further platelet aggregation
- Morphology of platelet ∆ due to ↑Ca2+, allows ↑SA for further activation
Aggregation
- Activated IIb/IIIa receptors → bind vWF/Fibrinogen
- Allows intraplate signalling
- Allows aggregation
- Amplified by ↑ADP, TXA2, dense granule release
- ADP also ↑ IIb/IIIa receptors
Version 1 Author: Krisoula Zahariou
Version 2
Definition
Platelets are one of the cellular components of blood, small cell fragments primarily involved in haemostasis. Platelets have a half-life of 4-12 days in blood before being removed by the reticuloendothelial system.
Formation – Thrombopoiesis
- Occurs in the bone marrow
- Pluripotent stem cells progressively differentiate and multiply under the influence of cytokines/growth factors:
- Pluripotent stem cells
- Common myeloid progenitor (CFU-GEMM)
- CFU-Meg
- Megakaryoblast – large nucleus containing multiple copies of the genome (occurs through endomitosis)
- Promegakaryocyte – even larger nucleus, some cytoplasmic granules
- Megakaryocyte – large cell with large nucleus, containing up to 32 copies of each chromosome.
- Platelets – formed by the budding and fragmentation of megakaryocyte projections. Each megakaryocyte produces ~5000 platelets.
- Thrombopoietin (TPO) is the major growth factor involved in platelet formation – promotes differentiation to megakaryocytes and the release of platelets from bone marrow. Produced mainly in the liver and kidney, but also within bone marrow.
- TPO can be degraded by platelets -> negative feedback
- IL-6 and IL-3 may also play important roles in thrombopoiesis
Structure
- Tiny discs 1-4 micrometres in diameter
- Organelles
- No nucleus. Functioning mitochondria, residual parts of the endoplasmic reticulum (i.e. the platelet dense tubular system) and Golgi body
- Cell membrane
- External glycocalyx – glycoproteins with specific functions (e.g. GP Ia-Iia). Repulses normal epithelium and promote attachment to damaged epithelium
- Specific surface receptors – e.g. Thrombin, ADP receptors
- Specific phospholipids involved in coagulation
- Contractile proteins – actin, myosin, and thrombosthenin
- Granules
- Alpha granules – contain Factor V, vWF, Fibrinogen, Platelet Factor 4
- Dense Granules – contain ADP, ATP, Calcium, Serotonin
Function
Haemostasis – Primary Function
- Formation of a platelet plug – adhesion-activation-aggregation
- Adhesion – the platelets adheres to the damage vascular surface (GP Ia-IIa -> collagen, GP Ib-V-IX -> vWF)
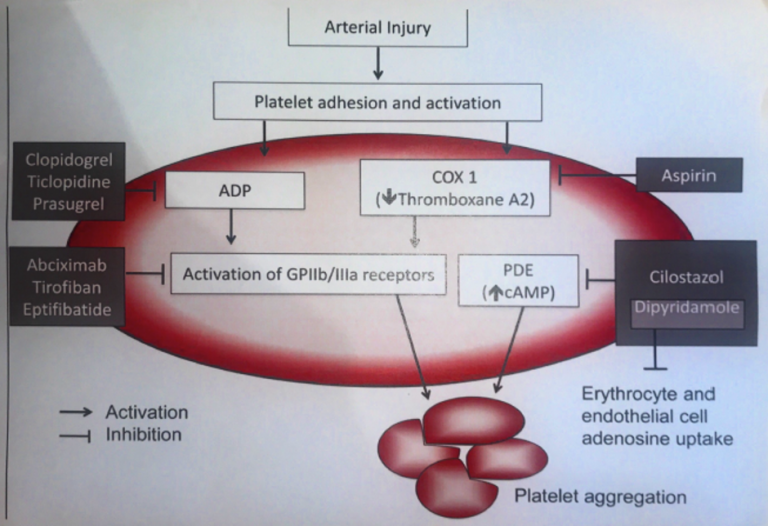
- Activation – GP VI + collagen -> activates the platelet -> granule release, morphology change, activation of the GP IIb-IIIa receptor, Thromboxane A2 (TXA2) production.
- Can also be activated by ADP, Thrombin, and TXA2
- Aggregation – activated platelets aggregate by binding to fibrinogen through GP IIb-IIIa, forming the platelet plug.
- Interaction with the coagulation cascade
- Platelet phospholipids and released Ca are crucial co-factors to many clotting factors
- Secrete Factor V (in alpha granules)
- Many of the steps of the coagulation cascade occur on the surface of the platelet (cell-based model)
- Platelets secrete and bind to fibrinogen (via GP IIb/IIIa)– helps form stable cross-linked fibrin clot
- Secretion of vasoactive substances (e.g. TXA2) – increases and sustains vessel spasm
- Clot retraction – contractile proteins within platelets assist in drawing the clot together
- Fibroblast invasion – platelets promote fibroblast invasion to clot, important for healing vascular injury.
Immune Function
- Innate immunity – express all 9 Toll-like receptors
- Immune regulatory role – not completely elucidated
Version 2 Author: Joshua McLarty