G3ii / 21A05 / 19B06: Outline the factors that determine CVP and explain how it is measured
21A05: Exam Report
Outline the factors that determine central venous pressure (60% marks) and explain how it is measured (40% marks)
57% of candidates passed this question.
This question examined a core area of cardiac physiology and measurement. Considering this, candidates overall, scored poorly in this section. There was a common misunderstanding around the relationship between cardiac output and CVP. A decrease in cardiac output (e.g. due to either decreased stroke volume or heart rate) will cause an increase in CVP as blood backs up in the venous circulation, increasing venous volume as less blood moves through to the arterial circulation; the resultant increase in thoracic volume increases central venous pressure. Several candidates confused the direction of their arrows, for example “increased right atrial compliance increases CVP”. Double negatives were used by several candidates which then resulted in the incorrect relationship described. (e.g., “arrow down compliance and arrow down CVP”). The measurement section should have included an explanation of the components of an invasive pressure monitoring system relevant to the measurement of CVP.
19B06: Exam Report
Outline the factors that determine central venous pressure and explain how it is measured.
18% of candidates passed this question.
It was expected that answers include central venous blood volume, central venous vascular compliance, intrathoracic pressure and tricuspid valvular function.
Good answers outlined how each of these factors determine CVP and whether it was increased or decreased. Many candidates incorrectly described the effect of venous return.
G3ii / 21A05 / 19B06: Outline the factors that determine CVP and explain how it is measured
Definition
- Venous Pressure = average blood pressure in the venous compartment
- CVP = the pressure in the thoracic vena cava near RA
- Normal CVP = 0 – 6mmHg (spontaneous, non-ventilated)
- CVP = Central Venous Volume / Central Venous Vascular Compliance
Use
- Veins are a low P, high capacitance vessel → P ∆ transmitted
- Reflects filling of RV
- Which by F – S definition determines SV
Cvp Waveform
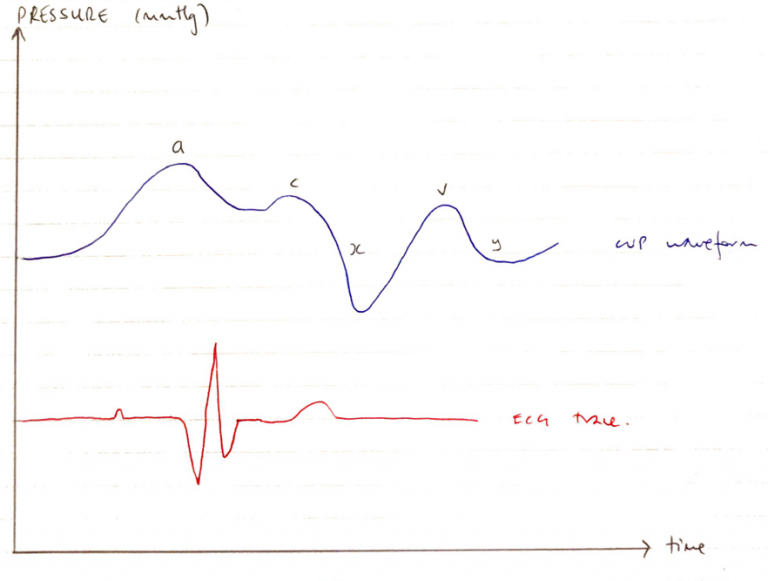
Wave
Event
ECG
a
Atrial contraction
Correlates with P wave
c
Cusp of tricuspid valve bulging backwards into atrium as RV contracts
Correlates with end of QRS
x
RV contraction → pulls down & ↓P in RA
Correlates with before T-wave
v
Valve is shut & atria is filling
Correlates with after T-wave
y
TV opens, blood rapidly fills ventricle ∴↓RAP
Correlates with before P wave
Determinants
Central Venous Blood Volume
Factors determining the rate of venous blood flow back to the heart:
Venous Blood Volume
Venous blood volume is dynamic and changing with
- CO: poor CO increases CVP
- RAAS: fluid retention increases CVP
- Position: supine increases CVP
Pressure gradient for venous return
- P gradient from veins → RA is main determinant of VR
- MSFP = average pressure of all pressures in the vessels
- P gradient for VR = MSFP – RAP = 7 – 1 = 6mmHg
Venous valves
- One way → prevents retrograde flow
Skeletal muscle pump
- Contraction/relaxation squeezes blood out of veins towards the heart → Increases CVP
Respiratory pump
- ∆ intrathoracic P
- INSP → intrapleural P ↓ – 5cm H2O to -8cm H2O
- This ↑ blood from veins into RA
Cardiac cycle
- Ventricle contraction → pulls TV downwards, lengthening atria → ↓RAP
- ∴ Promotes BF from veins into RA
Central Venous Vascular Compliance
- Compliance of large thoracic veins does not fluctuate much
- Major venous compliance change occurring in small veins outside of thorax
- Influenced by sympathetic NS; Symp → VenoC (decreased compliance) → increased promotes increase volume returning to Great Veins
Measurement
Non-Invasive: estimated by height of JVP, bedside echocardiography
Invasive: by the connection of one central line lumen to a pressure transducer (electrical) or fluid manometer (manual)
Equipment
- Central Venous Catheter
- Giving Set with Non-compressible fluid inflated to 300mmHg
- Allows Hydraulic Coupling
- 3 way tap
- Allows zeroing and blood sampling
- Pressure Manometer/Transducer
Mechanism
- Seldinger technique introduction of central venous catheter under ultrasound technique in full sterile precautions
- CXR to ensure correct positioning of catheter/monitor for complications
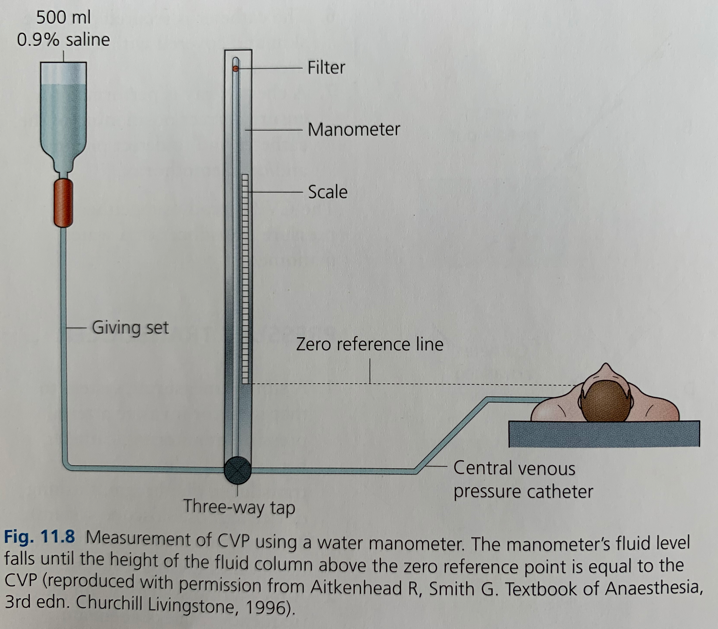
Manometer
3 way tap connects manometer to IV set on one side & patient on other side
3way tap is turned off to the patient to allow the manometer column to fill with fluid
Then 3 way tap turned off to the fluid bag (open to patient & manometer) and the fluid level falls to the level of CVP and read on the manometer scale (cmH20)
The manometer uses a balance of forces; downward pressure of fluid (determined by density and height) v pressure of central venous system (determined by hydrostatic and recoil forces
Pressure Transducer
Pressure transducer consists of a diaphragm and strain gauge, Signal Processor Cable and Monitor
Transducer is placed at level of RA
Transducer is connected to CVP catheter via fluid filled tubing
3 way tap closed to patient → transducer ‘zeroed’ to atmospheric P
3 way tap is then closed to room air and open between patient & transducer → continuous CVP reading (mmHg)
Electrical Signal from transducer is transmitted for filtering, amplification, analysis and display on screen as a Pressure v Time waveform
Error
Air bubbles/embolus
Catheter position
Both techniques require zeroing at the level of the RA to eliminate the effect of hydrostatic pressure on the CVP value
- Author: Krisoula Zahariou