F12i / 21A17 / 14A07: Principles of pulse oximetry
21A17: Exam Report
Describe the principles of measurement of arterial haemoglobin O2 saturation using a pulse oximeter (60% marks). Outline the limitations of this technique (40% marks).
74% of candidates passed this question.
Most candidates provided a reasonable structured sequence of how a pulse oximeter generates a value. Nearly all candidates described the Beer-Lambert laws correctly, but few specifically described the basic principles of absorption spectrophotometry. Most candidates had a reasonable list of extrinsic factors that can interfere with pulse oximeter performance, but few described the intrinsic/inherent limitations of the device that can cause SpO2 to be different to SaO2, such as functional versus fractional saturation.
14A07: Exam Report
Outline the principles underlying pulse oximetry. ( 80% of marks) Briefly describe the effect of an elevated level of the following upon pulse oximetry values. (20% of marks) a) Carboxyhaemaglobin b) Methaemaglobin
34% of candidates passed this question.
Explanation of several crucial principles was expected for a good answer. These would include that Haemoglobin can be measured and quantified with a light absorbance technique; based on the Beer Lambert law (a description of this was required).
In addition, oxygenated haemoglobin must be distinguished from reduced haemoglobin (the 2 dominant species of Hb) and that the oximeter determines pulsatile from non pulsatile blood. The oximeter accounts for ambient light and that “R”, a ratio of absorbances during pulsatile and non pulsatile flow is calculated and compared within a computer algorithm to standardised values of SaO2 to deliver a final value.
Mention of limitations was not required except to answer the second part of question. Common omissions included failure to describe accurately the Beer Lambert Law, and no explanation of how pulsatile component was detected, or ambient light accounted for. Many candidates understood the clinical inaccuracy associated with CO and Met HB, but failed to identify the spectrophotometric reason and application of the R value for this discrepancy.
F12i / 21A17 / 14A07: Outline the principles underlying pulse oximetry (80 marks) + Briefly describe the effect of an elevated level of the following on pulse ox values (20 marks)
Definitions
- Pulse oximetry = a spectrophotometric technique used to measure O2 sat in arterial blood
- Normal Value > 92%
Beer-Lambert Law
- The physical principle underlying pulse oximetry
- Beer’s Law: light transmission 1/∝ Concentration
- Lambert’s Law: light transmission 1/∝Path Length
∴ BL LAW = light transmitted through a substance ↓exponentially with ↑distance & concentration
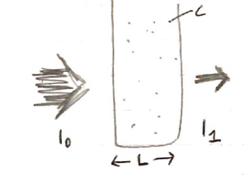
When light of intensity (I0) passes through a substance, it is absorbed & the beam exiting the substance has ↓light intensity (I1)
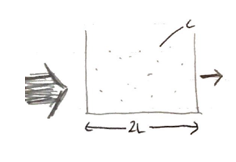
When path length doubles, twice the amount of light absorption also occurs & ↓l1 twice as much
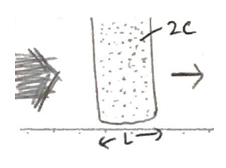
When [ ] (C) doubles, again twice the absorption occurs with ↓l1
Principle
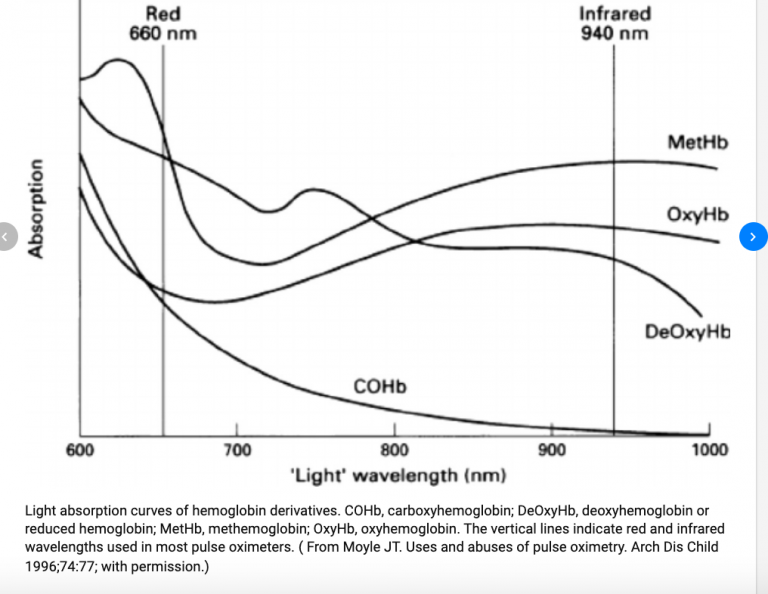
- Pulse ox exploits the difference in absorption of light by oxy & deoxy Hb
- OxyHb absorbs more Infrared (IR) light → 940nm
- DeoxyHb absorbs more red light → 660nm
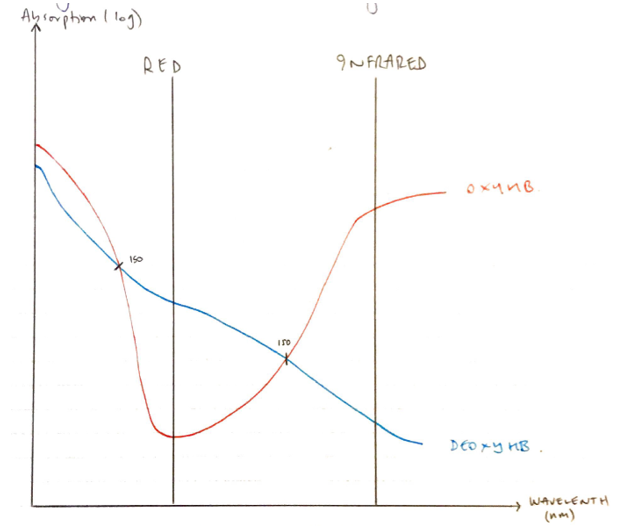
ISOSBESTIC POINTS = where 2 substances absorb light at the same extent
- When light at these 2 different wavelengths is transmitted through Hb-containing solutions, it is possible to solve an equation to calculate the ratio of oxy:deoxy Hb & give a % oxygen saturation
- 2 separate LEDs transmit light
- RED LIGHT (660nm)
- IR (940nm)
- Sensor detects light, but not wavelength
- ∴machine has to know which light is flashing
- It goes in a sequence:
- Red light
- IR light
- Pause (to analyse ambient light)
- Photocell detection on opposite side of finger reads light intensity
- When ambient light has been filtered, the signal consists of AC & DC component
- DC = skin, muscle, bone, venous BF
- AC = arterial BF
- All pulse ox assumes only the pulsatile absorbance is arterial blood
- The AC/DC ratio is calculated:S
\( \Large \textbf{R = } \normalsize \frac{\text{ (AC Abs/DC Abs) Red }}{\text{(AC Abs/DC Abs) IR}} \)
- R corresponds to SpO2:
- SpO2 100% = R = 0.4
- SpO2 85% = R = 1
- SpO2 0% = R = 34
- Derived from volunteer experimental data
Set Up
- Biological variable: O2 saturation
- Peripheral probe:
- 2 LED emitting lights
- A photodetector on the other side
- Integrator: microprocessor which analyses both AC + DC to calculate the ratio
- Output:
- Graphic display giving O2 saturation as a number & plethysmography waveform
- Pitch for SpO2 value
Limitations
- Lag time → 10s ear, 60s finger
- Does not measure tissue oxygenation, just % saturation of Hb
Errors
Sensor
- Lag time → 10s ear, 60s finger
- Does not measure tissue oxygenation, just % saturation of Hb
Processing
- Lag time → 10s ear, 60s finger
- Does not measure tissue oxygenation, just % saturation of Hb
Abnormal Hb
MetHb
- Occurs when Fe2+ of Hb is oxidised → Fe3+
- MetHb has absorption peaks at 630 nm and 960 nm
- At 660 nm and 940 nm, red and infrared light are absorbed at a 1:1 ratio
- Results in R ≈ 1
- R = 1 corresponds to SpO2 85% by pulse oximetry conversion algorithm
- SpO2 reads 85%
- ∴patient can be hypoxic &sat is reading 85% OR patient can be SpO2 100% and sat is reading 85%
- MetHb impairs O2 delivery because:
→ MetHb is less able to bind O2
→ Causes normal Hb ODC to shift L) which impairs O2 unloading at tissue level
CO Hb
- Absorbs identical to HbO2 660nm
- ∴photodetector reads sum of HbO2 + COHb
- ∴over-estimates sats
Dyes
- Methylene blue → peak light absorbption of 668nm
- Very closely corresponds to light absorbance peak of deoxyHb (660nm)
- The MB absorbs most of the light giving a false estimate of the % OxyHb
- Thus → underestimates sats
Blood Flow
Poor perfusion = ↓AC/DC ratio
- R approximates 1 ∴SpO2 = 85%
- Inaccuracy compounded by ↑noise (VC, hypothermia)
Pulsatile Venous BF
- g. Severe TR
- Involved in R calculation
ODC Relationship to SpO2
- At STD temp & pH (37°, 7.4)
- Sats correspond to following pO2 by ODC
- SpO2 97% → pO2 100
- SpO2 91% → pO2 60
- SpO2 75% → pO2 40
- But ODC can be shifted L/R by temp, pH, 2,3 DPG
- Foetal Hb → L) shift
- In flat upper part ODC > 98% the pO2 can be anything!
- In steep part → SpO2 < 80%, it is inaccurate pO2 measurement
- Author: Krisoula Zahariou