L2i / 22A13: Compare and contrast the pharmacology of Suxamethonium and Rocuronium
22A13: Exam Report
Compare and contrast the pharmacology of Suxamethonium and Rocuronium
75% of candidates passed this question.
Suxamethonium is a level 1 drug and therefore requires a detailed knowledge of the drug from a PK and PD perspective as well as consideration of important side effects and considerations when used.
The examiners commented that a table structure with the structured pharmacology headings and clear concise facts was the best way to approach this question. Answers that scored poorly often displayed incorrect facts, limited appreciation of side effects and vague statements on the pharmacological particularities of this drug. For example, muscle relaxants are major culprits for anaphylaxis in hospitals, and nuanced facts about this were generally missing from candidate’s answers.
L2i / 22A13: Compare and contrast the pharmacology of Suxamethonium and Rocuronium
Suxamethonium (succinylcholine)
Rocuronium
Class
Suxamethonium (succinylcholine)
- Depolarising muscle relaxant
Rocuronium
- Nondepolarizing muscle relaxant
Chemistry
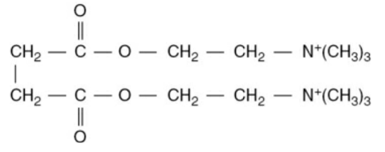
Suxamethonium (succinylcholine)
- Two molecules of Ach joined back-to-back joined by their acetyl groups
Rocuronium
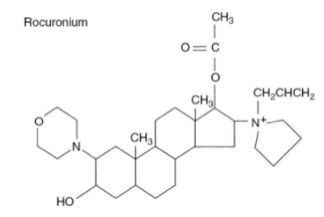
Aminosteroid , monoquaternary (low potency)
Use
Suxamethonium (succinylcholine)
- Rapid and profound NMB e.g. endotracheal intubation
- Modification of seizures post ECT
Rocuronium
- Facilitation of endotracheal intubation in routine + modified RSI
- For control of ventilation
Presentation
Suxamethonium (succinylcholine)
CCSI @ 4oC 50mg/mL
- One ampoule contains 2mg in 10mL (1 dose for a 70kg person)
Rocuronium
CCSI @ 4oC 10mg/L
Dose
Suxamethonium (succinylcholine)
- IV: 1-2mg/kg (RSI)
- IM: up to 2.5mg/kg
Rocuronium
- IV 1mg/kg (RSI)
- (infusion 9-12 microg/kg)
Onset
Suxamethonium (succinylcholine)
30-60s (indicated by fasciculations)
Rocuronium
60-90s
Duration
Suxamethonium (succinylcholine)
3-10 min
Rocuronium
35min
MoA
Suxamethonium (succinylcholine)
AChR (nicotinic) competitive agonist.
Mimics Ach -> binds receptor and gives a prolonged membrane depolarisation
- Inactivates voltage sensitive Na+ channels within 1-2mm
- Effect lasts longer than Ach as hydrolysing enzyme not present at NMJ as its hydrolysing enzyme (plasma or pseudocholinesterase) is not present at the neuromuscular junction
Phase I block: initial block
Phase II block: after further doses of drug, block becomes prolonged and characteristic become similar to those of non-depolarising block (likely due to presynaptic feedback)
Rocuronium
Competitive antagonist at ACHR on postsynaptic membrane (also some presynaptic activity)
- Bind to the alpha subunit of the nicotinic acetyl choline receptor
CNS
Suxamethonium (succinylcholine)
Increased IOP (significant in globe trauma), increased ICP
Rocuronium
Does not cross BBB, reduced incidence IOP
Resp
Suxamethonium (succinylcholine)
- Apnoea
Rocuronium
- Apnoea
- histamine release (can cause bronchospasm but very uncommon)
CVS
Suxamethonium (succinylcholine)
- Bradycardia
- Ventricular arrhythmias
Rocuronium
Minimal (vagolytic in large doses with 10% increase in HR and MAP)
GIT
Suxamethonium (succinylcholine)
Increased intra-abdominal pressure and reduced LOS tone (= aspiration risk)
Rocuronium
Metabolic
Suxamethonium (succinylcholine)
Increased serum K+ (0.2-0.4mmol/L) -> significantly increases in burns, muscle denervation (e.g. spinal cord injury), renal failure
Rocuronium
A/E + Toxicity
Suxamethonium (succinylcholine)
Most common to least common:
- Myalgia (young females)
- Cardiac arrhythmias
- Sinus or nodal bradycardia, or ventricular arrythmias
- Bradycardia is most common in paediatric patients with a 2nd dose
- Hyperkalaemia
- In normal individuals, transients increase of ~0.5mmol/L
- This can be enough to cause a cardiac arrest in patients with high baseline K+ e.g. renal failure
- Increased IOP
- 10-15mmHg, but transient
- Use cautiously in open eye injury
- Concurrent thiopentone offsets this rise
- Increased intragastric pressure
- By ~10cmH2o
- Offset by increase in LOS tone
- Anaphylaxis (1:2000)
- Sux apnoea (prolonged neuromuscular block)
- Reduction in plasma cholinesterase activity due to genetic variability or acquired conditions
- Single locus point mutation on chromosome 3, making up 10 genotypes (see below)
Malignant hyperthermia (1:20,000)
Rocuronium
- Pain on injection
- Fatal anaphylactoid reactions (rare)
- 1:2500
- Cross sensitivity with vecuronium and pancuronium
Contraindications
Suxamethonium (succinylcholine)
- Patients with hyperkalaemia
- Severe muscle trauma
- Hx of malignant hyperthermia or sux apnoea
- Burns of >10%
- Spinal cord trauma
- Avoid for 24hrs to 18 months post
- Patients with muscle disease
Rocuronium
Elimination is NOT altered by renal failure but IS altered by hepatic failure
A
Suxamethonium (succinylcholine)
IV (and IM/subling)
Rocuronium
IV
D
Suxamethonium (succinylcholine)
Vd 0.25L/kg
PB 30%
Rocuronium
- Vd 0.2L/kg
- PB 10%
M
Suxamethonium (succinylcholine)
Rapidly hydrolysed by plasma esterase’s into succinic acid and choline (only 20% reaches NMJ)
Rocuronium
<5% hepatic metabolism. No metabolites in plasma/urine
E
Suxamethonium (succinylcholine)
<10% excreted in urine unchanged
T1/2 45s
1st order kinetics
Rocuronium
Hepatobiliary
30-40% bile, 10-30% urine
T1/2 90 min
3 exponential phases
Reversal
Suxamethonium (succinylcholine)
- Nil effective reversal
Rocuronium
- Neostigmine + glycopyrrolate
- Sugammadex
Duration of block prolonged by
Suxamethonium (succinylcholine)
Genetic factors
- 4 alleles making up 10 genotypes
- Usual (normal): Eu
- Atypical (dibucaine-resistant): Ea
- Silent (absent): Es
- Fluoride resistant: Ef
- Mutations occur in 4% of population
- Prolong block to varying degrees
- Separated by dibucaine number
Acquired factors
- Factors associated with a reduction in plasma cholinesterase’s/pseudocholinesterase’s
- Pregnancy
- Liver disease
- Renal failure
- Cardiac failure
- Thyrotoxicosis
- Cancer
- Drugs
- Substrates or inhibitors of AChE
- E.g. metoclopramide, ketamine, OCP, lithium, lidocaine, ester local anaesthetics, edrophonium, neostigmine
Rocuronium
- Hypermagnasaemia
- Hypo kalaemia/calcaemia
- Hypothermia
- Low protein
- Dehydration
- Acidaemia and hypercapnia
Summary of key differences
- Suxamethonium is a depolarising neuromuscular blocker, rocuronium is a non-depolarising neuromuscular blocker
- Suxamethonium has a faster onset and offset than rocuronium
- Suxamethonium has an increased side effect profile and more contraindications
- Rocuronium much less likely to cause increased intracranial pressure, hypertension or intraocular pressure
- Suxamethonium can cause hyperkalaemia
- Rates of anaphylaxis are similar, however, there is more of a risk with suxamethonium (clinically you will see more Rocuronium anaphylaxis as it’s use is more common)
- Rocuronium is not metabolised, suxamethonium is rapidly metabolised
- There is no effective reversal for suxamethonium, rocuronium can be more reliably reversed with anticholinesterases and suggamadex
More information on Suxamethonium
Suxamethonium adverse effects mnemonic:
3 major
- Anaphylaxis
- Suxamethonium apnoea
- Malignant hyperthermia
3 minor
- Hyperkalaemia
- Bradycardia
- Myalgias
3 pressures
- Raised intraocular pressure
- Raised intracranial pressure
- Raised intragastric pressure
Sources
- Peck and Hill. Pharmacology for Anaethesia and intensive Care. 4th edition ,Chapter 12
- Scath and Smith. Drugs in anaesthetics and Intensive Care. 5th edition
- Flood and Rathmell. Stoelting’s Pharmacology and Physiology in anaesthetic practice. 6th edition, Chapter 12
- Propofol Dreams: https://propofoldreams.wordpress.com/
- Ketamine nightmares: https://ketaminenightmares.com/
Author: Erin Maylin