O1ii / 22A14 / 14A03: Vomiting
22A14: Exam Report
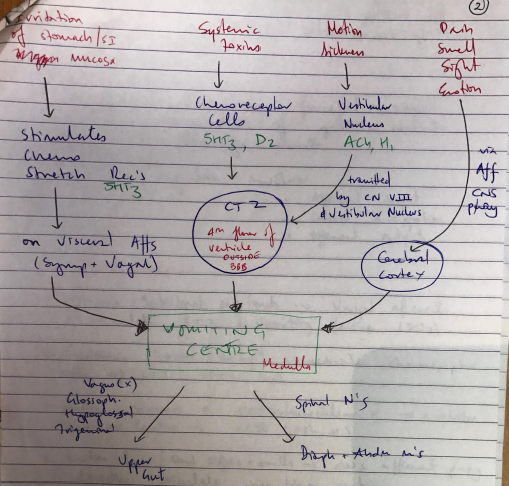
Describe the neural integration of vomiting, highlighting the site and mechanism of action of antiemetics
60% of candidates passed this question
The examiners commented that a well-drawn and labelled diagram was a very useful adjunct to answering this question.
Consideration of stimulus, sensors, integrators/processors, and effectors was also useful to ensure that all components of the question were covered by a candidate’s answer.
Incorrect facts or a lack of detail about the various receptors and their locations was a common theme in answers that scored poorly.
Classes of antiemetics, with specific drugs given as examples, were expected to gain marks.
14A03: Exam Report
Describe the neural integration of vomiting. (60% of marks) Describe the pharmacology of ondansetron. (40% of marks)
58% of candidates passed this question
Candidates who failed the question did not answer the actual question. They did not discuss the neural integration but instead listed various inputs into the CTZ and vomiting centre.
It was expected candidates could detail the pathways involved (afferent and efferent limbs) and describe the relationship with the coordinating centres.
For example, afferent pathways to the vomiting centre include stretch and chemoreceptors located throughout the GIT via vagal and sympathetic nerves, pharyngeal touch receptors via glossopharyngeal nerves etc.
Again structuring pharmacology answers was often poor.
O1ii / 22A14 / 14A03: Describe the neural integration of vomiting (60 marks). Describe the pharmacology of ondansetron (40 marks)
Definition
Vomiting = involuntary, forceful + rapid expulsion of gastric contents through mouth
- Neutral integration involves:
- Afferent input
- Central integration
- Efferent outputs
1) Sensory Inputs
- Stomach/intestinal irritants → vagal afferents → stimulate CTZ & vomiting centre (5HT3)
- Systemic toxins (drugs) → activate chemoreceptor cells of CTZ (5HT3, D2)
- Motion sickness → vestibulocochlear n. → activates vestibular centre → CTZ (ACh, H1)
- Emotion/pain/foul sights & smells → CNS afferent pathway → directly stimulates VC
- Head injury → direct central effect on VC
2) Central Integration
- CTZ
- Located on 4th floor ventricle, medulla, outside BBB
- Relays stimuli to vomiting centre
- Receptors for all emetic stimuli (M1, D2, 5HT3, NK1, H1)
- Vomiting Centre
- Located in Medulla
- Mainly muscarinic receptors
- Activated by:
- CTZ impulses
- Higher brain centres
- Visceral afferents (directly)
3) Efferent Outputs
- Brainstem causes abdominal contraction & expulsion of gastric contents via:
- Vagus, glossopharyngeal n. → upper gut
- Spinal nerves → diaphragm + abdominal m’s
Mechanism:
deep inspiration + closure of glottis
↓
LOS relaxation, reverse peristalsis
↓
Strong abdominal m. contraction
↓
Diaphragm descends → ↑↑↑abdominal P
↓
↑pressure on stomach forces contents into oesophagus
↓
UES relaxation & contents expelled through mouth
Classes of anti-emetics
Class
Example
Class
D2 Antagonist
Example
- Phenothiazine
- Chlorpromazine
- Prochloperazine
- Butyrophenones
- Droperidol
- Domperidone
- Benzamides
- Metoclopramide
Class
Anticholinergic
Example
- Hyoscine
- Atropine
Class
5HT Antagonis
Example
- Tropisetron
- Ondansetron
Class
H1 Antagonist
Example
- Phenothiazine
- Promethazine
Class
Other
Example
- Steroids
- Cannabis
- Propofol
- Benzodiazepines