F2i / 22B04: Control of Ventilation Increase RR
22B04: Exam Report
List the physiological factors which increase respiratory rate and explain their mechanism
22% of candidates passed this question.
It was expected that candidates would provide not only a list of factors which increase respiratory rate but to give physiological reasoning behind each mechanism.
Providing a list of factors was not sufficient for a pass. Vague, imprecise answers attracted fewer marks.
A request to explain a mechanism requires the candidates to write a comprehensive physiological reasoning.
Many candidates did not demonstrate a comprehensive understanding of these mechanisms. Most answers failed to include all the stimulants of respiratory rate, especially the non-chemical controls.
Many answers were not structured or structured in a way that meant they missed many of the mechanisms or that they repeated the same information through the answer which used time but failed to gain additional marks.
F2i / 22B04: Control of Ventilation Increase RR
Respiratory Rate
- Time taken for complete INSPIRATION, followed by EXPIRATION
- Measured as no. of breaths / min
- At rest 12 – 16bpm
Control of Ventilation
- Respiratory centre in Medulla
Factors Altering to ↑RR
Send information to resp centre of Medulla
- Chemoreceptors: ↑pCO2, ↓pO2, ↑H+
- Higher centres: pain, fear, anxiety
- Lung receptors: irritants, bronchoconstriction
- Baroreceptors: ↓BP
- Nociceptors: Pain
- Thermoreceptors: ↑Temp
- Joint/Muscle receptors: ↑Limb movement
- Extremes: ↑[progesterone]
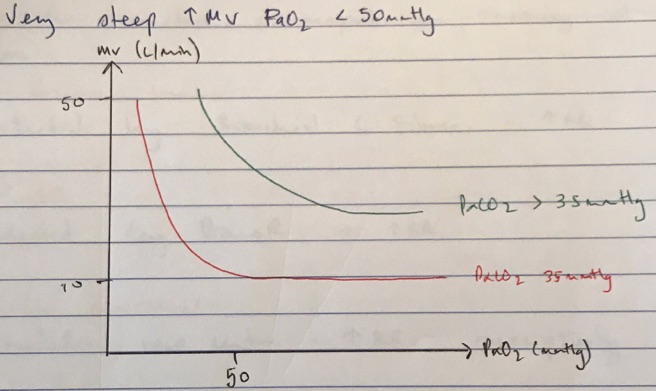
↑pCO2
- Detected by central (95%) & peripheral chemoR (5%) → response to ↑pCO2
- Sensitive minute-by-minute detection
- Peripheral work faster but greater overall response from Central ChemoR
- Central chemoR detects Brain ECF [H+]
- ↑CO2 → ↑CO2 CSF → diffuses across BBB → converted
- CO2 + H2O ⇄ H2CO3 ⇄ H+ + HCO3- → ↑[H+] → ↑afferent output of central chemoR to resp centre → ↑MV
- sensitive to ∆pCO2 because CSF has less buffering capacity cf. blood because ↓[protein] with ↑MV 2 – 3L/min for every 7mmHg ↑CO2
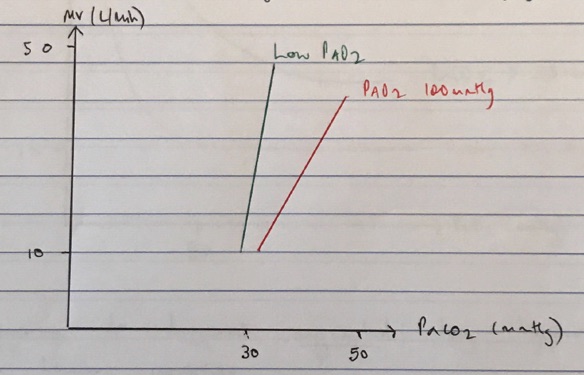
↓pO2
- Peripheral chemoR = high rate of perfusion = small A-V difference → detected + rapidly respond to ∆pO2
- Stimulated by O2 tension NOT CONTENT
- ↓pO2 = ↓intracellular ATP = ↑intracellular Ca2+ = ↑firing T1 glomus cells = ↑firing Glossoph. + Vagus nerves → resp centre → ↑MV
- Response to hypoxia augmented by hypercarbia
- Non-linear response
↑H+
- Peripheral detected by peripheral ChemoR (CAROTID BODY)
- pH sensitive K+ channels or peripheral chemoR
- ↓intracellular ATP = ↑firing of afferents to resp C = ↑MV
- Can also directly activate Resp Centre (Vagal input)e. DKA ↓pH, ↓pCO2, but ↑↑↑RR
- If pH drops low enough, BBB will become permeable to H+ & central chemoR respond
Pain, fear, anxiety
- Stimulate irritant receptors of upper airway = ↑RR
Toxins, mucous
- Detected by bronchial C fibres = ↑RR
↓BP
- Detected by BaroR → ↑RR
Limb movement
- Stimulates resp centre = ↑RR pre-emptively
Pregnancy
- ↑[Progesterone] = ↑MV
↑Temp
- Detected by thermoreceptors = ↑RR