V1i / 23A18: Explain the respiratory changes that occur at term in pregnancy
23A18: Exam Report
Explain the respiratory changes that occur at term in pregnancy
43% of candidates passed this question.
Good answers addressed the following in an ordered way: anatomic changes (including to airway, thoracic dimensions, dead space, airways resistance); what changes there are to respiratory volumes, capacities, and compliance; what happens to oxygen consumption and oxygen tension; and the acid-base changes that occur.
Good answers didn’t just list these changes, but also provided an explanation for them. Few candidates mentioned the changes in oxygen tension and oxygen consumption, and why these occurred
V1i / 23A18: Explain the respiratory changes that occur at term in pregnancy
Physiological changes occur to assist development of the foetus and prepare mother for labour and delivery.

Airway Anatomy
- Capillary engorgement
- Increase in tissue friability
- Oedema of oropharynx/larynx/trache
- = difficult intubation and increase risk of bleeding
- The enlarged breast tissue further exacerbates airway difficulty and may require use of a short handle
Thoracic Dimension
- Progressive ligamentous laxity peaks at 37 weeks due to the hormone Relaxin
- Diaphragm is displaced upwards 4cm by gravid uterus
- Increased thorax circumference by 8cm
- Increased AP diameter 2cm
- Increase in thoracic dimensions as chest height becomes smaller to maintain TLC
Dead Space & Ventilation
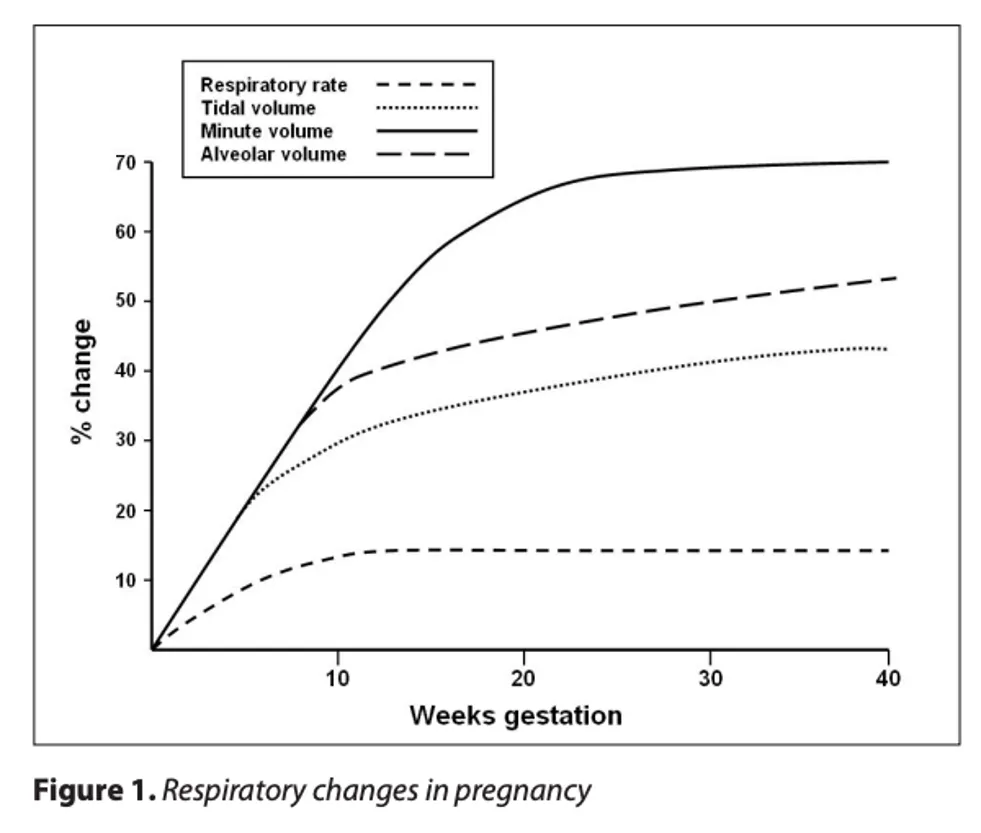
- 1st trimester sees an increase in MV (Vt >> RR) due to increase [Progesterone] and increase CO2 production
- The amount of dead space remains the same and overall results in increased alveolar ventilation by 30-50%
- Matched by an increase in CO, this results in an increase in alveolar ventilation 45% over baseline (reducing the ETCO2-PaCO2 gradient)… this is incompletely metabolically compensated with an increase in pH 0.02-0.06
- The reduction in PaCO2 will facilitate diffusion of CO2 out of the placenta
Raw
- This qn states at term → respiratory resistance increases while respiratory conductance decreases during pregnancy
- However, during late pregnancy hormonally induced relaxation of tracheobronchial tree smooth muscles reduces airway resistance
- Throughout pregnancy spirometry remains within normal limits with:
- FEV1
- FVC
- FEV1/FVC
- It is the lung volumes that undergo major changes
Respiratory Volumes, Capacities
Decrease
- ERV 20%
- RV 20%
- FRC 20% (supine 70%)
- Expiratory capacity
Increase
- Inspiratory capacity
- Vt
- No change in CC
Increase in Inspiratory Capacity to maintain stable TLC
Despite upward diaphragmatic displacement, the diaphragm moves with greater excursion and much more efficiently than the thorax
Compliance
Pulmonary static & dynamic compliance, diffusion capacity and static lung recoil pressure do not change in pregnancy
Chest wall compliance foes reduced and is much worse in the lithotomy position
O2 Consumption
O2 consumption & BMR increase
The reduction in FRC coupled with high metabolic rate = reduced O2 reserve
Oxygen Tension
Due to the increased Minute Ventilation PCO2 falls to 27-32mmHg
During labour PCO2 falls further with each contraction
Following hyperventilation and reduced PCO2 the PaO2 increases 101-104mmHg at third trimester
Acid Base
- Despite hyperventilation & resp alkalosis the pH remains only slightly alkalotic 7.40-7.47 due to renal compensation & excretion of bicarboniate