F12i / 23B01: Explain why the oxygen-haemoglobin saturation value derived by a pulse oximeter (SpO2) could be different from the measured arterial value (SaO2)
23B01: Exam Report
Explain why the oxygen-haemoglobin saturation value derived by a pulse oximeter (SpO2) could be different from the measured arterial value (SaO2)
32% of candidates passed this question.
This question required candidates to identify that the measured arterial value (SaO2) was the gold standard to which the limitations of the pulse oximeter should be compared.
A detailed description of the intrinsic and extrinsic factors of potential sources of difference of the SpO2 measurement was then expected. Intrinsic factors included wavelengths used, pulse added absorbance, derivation of the SpO2 value and time delays.
Extrinsic factors where largely patient and environment related including light pollution, poor peripheral perfusion for various reasons, probe location variances and probe artefact.
F12i / 18A08: Explain why the oxygen-haemoglobin saturation value derived by a pulse oximeter (SpO2) could be different from the measured arterial value (SaO2)
Introduction
- SaO2 = true arterial oxygen saturations measured using co-oximetry with a blood gas machine – the reference standard
- SpO2 = Arterial saturations calculated using pulse oximetry to determine the “R value” which confers to a SaO2 value during healthy volunteer studies
- Provides an estimation of the true “SaO2”
- Accuracy decreases with lower SpO2 (not validated < SpO2 75%)
- SpO2 can be different to SaO2 due to intrinsic differences in its methodology and due to extrinsic factors
Intrinsic Factors
Wavelengths used and functional versus fractional saturations
- Both methods use light absorbance spectroscopy
- The Beer-Lambert law states that the amount of light absorbed by an absorbing substance is proportional to its concentration and the length travelled by the light. Different Hb species have different light absorption spectra
- DeoxyHb absorbs at a peak 660nm (red) wavelength; oxyHb at 940nm (IR).
- In co-oximetry multiple wavelengths are shone through the sample continuously, and the proportion of many Hb species can be determined.
- In pulse oximetry, only 2 wavelengths (660nm and 940nm) are shone through the finger and a photodetector on the other side measures how much light gets through. The concentration of the relevant haemoglobin species is inversely proportional to the amount of light of the relevant wavelength reaching the detector.
- The amount of light absorbed in total represents a summation of the non-pulsatile tissues (skin, soft tissue, bone, venous blood; DC) with the pulsatile signal (arterial blood; AC)
- The AC component is only 1-5% of the total signal
- To determine only the arterial (pulsatile) signal, the non-pulsatile signal (from venous blood and tissue) is eliminated by using an emitter which cycles between the wavelengths and turns “off” at 400-900Hz. The microprocessor uses the “off” time to correct for ambient light. An equation is then used which corrects for the non-pulsatile signal, generating an “R” value which has been equated to an SpO2 value by healthy volunteer studies
- R = AC(660nm)/DC(660nm) / AC(660nm)/DC(660nm)
- Where AC is the alternating current and DC is the direct current.
- R=0.4 relates to SpO2 100%, R=1 relates to SpO2 85%
- The SaO2 can therefore be different to the measured SpO2 due to measuring fractional saturations rather than functional saturations.
- In co-oximetry, multiple light wavelengths are used to determine the concentrations of multiple Hb species (HbO2, DeoxyHb, COHb, MetHb, fetal Hb) and SaO2 (fractional saturations) = HbO2 / (HbO2 + DeoxyHb + COHb + MetHb, fetal Hb)
Time delays
- If the arterial sample is not processed immediately, then the SaO2 may fall and cause it to be lower than the SpO2. This is due to leukocyte larceny (ongoing use of O2 by WBC in the sample), and is more common in leukaemic patients
- The site of the SpO2 probe will determine how quickly a desaturation becomes evident, time delay to ear probe ~10s and time delay to finger probe ~60s
- Additionally, the SpO2 provides a continuous reading, whereas the SaO2 represents a snapshot in time. Therefore the values will be different in those with highly variable arterial oxygen saturations – for example in patients with sleep disordered breathing
Low saturations
- The R value generated by pulse oximetry was only calibrated in healthy volunteer studies to be accurate down to 75%, therefore if the SpO2 is lower than this, the accuracy of pulse oximetry falls, and the value is more likely to be different to SaO2
Extrinsic Factors
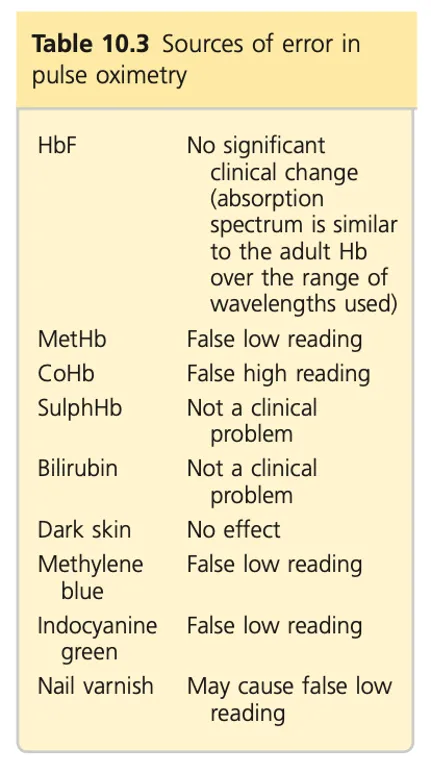
- Abnormal Hb species
- In the presence of significant concentrations of other Hb species, functional sats and therefore SpO2 become less accurate
- CarboxyHb: Absorbs at 660nm at similar amount to oxyHb. Therefore SpO2 represents false summation of oxyHb and carboxyHb, So if levels of carboxyHb are high, SpO2 could be falsely normal where SaO2 is low.
- MetHb: Absorbs at both 660nm and 940nm, so with high MetHb concentrations, “R” trends towards 1, therefore SpO2 trends towards 85%. Therefore will overread if SaO2 <85% or underread if SaO2 >85%.
- Reliance on pulsatile flow
- Due to relying on determining the pulsatile signal, pulse oximetry can be lower than SaO2 in:
- Non-pulsatile arterial flow e.g. poor peripheral perfusion, ECMO, ,
- Pulsatile venous flow e.g. Severe tricuspid regurgitation, high airway pressures, Valsalva manoeuvre
- Due to relying on determining the pulsatile signal, pulse oximetry can be lower than SaO2 in:
- Bright ambient light can cause SpO2 to under-read and have poor signal
- Movement artefact causes poor signal to noise ratio and pulse oximetry will read lower than SaO2. The SpO2 will try to correct this by averaging the sats over the previous 10s
- Poor signal will cause pulse oximeter to under-read e.g. Raynaud’s, poor perfusion – pulse oximeter will increase gain until it gets good signal
- Accuracy falls significantly when SBP <80mmHg because the AC component of the signal falls
- Blue nail polish will cause an increase in absorbance of red light at 660nm therefore causing an erroneous increase in deoxyHb and therefore it will read lower than the SaO2 value
- Skin pigmentation – higher discrepancy between SpO2 and SaO2
- IV dyes e.g. methylene blue / indocyanide green. Especially methylene blue, has a peak absorbance at 670nm, so absorbs a lot at 660nm so can cause SpO2 to underread.

Author: Alex Ashby