G4iii / K1iii / 23B14 / 21A20 / 14A14: Cerebral Blood Flow
23B14: Exam Report
Describe the physiological factors that influence cerebral blood flow?
56% of candidates passed this question.
Cerebral Blood Flow is result of CPP/CVR. The brain defends a relatively constant high blood flow via multiple auto-regulatory processes that influence cerebral vascular resistance.
This question required an in detail description of the physiological factors that alter CBF. Autoregulation via the myogenic and metabolic mechanisms, the difference between grey and white matter due to metabolic variation, the role of pCO2 and O2, sympathetic nervous system and temperature was expected. A “describe” question requires not only the factors that influence CBF but how and why, so detail is required.
Whilst the monroe kellie doctrine does describe changes in blood flow this is only important at extremes of intracranial pressure when these normal autoregulatory mechanisms are exceeded, as such it was not part of the answer to this question.
21A20: Exam Report
Outline the physiological factors that influence cerebral blood flow
19% of candidates passed this question.
Overall, this question was poorly answered with a high failure rate. A good answer gave a normal value, iterated that CBF is held relatively constant by autoregulation, and proceeded to divide factors affecting CBF into categories with an explanation/description of each. Those factors with the greatest influence were expected to have more accompanying information (e.g., pressure/myogenic autoregulation, metabolic). Systemic factors such as MAP, O2, CO2 were expected to be mentioned with detail of the impact (i.e., key values, relationships demonstrated with a description and/or labelled graph). Local factors within the brain such as H+ concentration/pH, metabolic activity (including the impact of temperature, inclusion of mediators, regional variation based on activity & grey versus white matter) were also expected to be mentioned. Few answers mentioned impact of pH change independently of CO2. Few answers mentioned how CO2 changes the pH of CSF and that over time, this impact is buffered/reduces. The role of the sympathetic nervous system was required to be mentioned although not explored in detail (although many answers overstated the importance of the SNS on CBF or gave a simplistic concept such as increased SNS activity increases CBF). Many answers focussed on descriptions of the Monro-Kelly doctrine and ICP to the exclusion of the aforementioned factors or included detail on factors influencing MAP which were not required (and irrelevant when within the autoregulation range). Many answers were simplistic: e.g., increase MAP increase CPP therefore increase CBF, or by stating CO2/O2 without mentioning a relationship or the limits/patterns of the relationship. Many answers failed to separate the effect of systemic PaO2 and PaCO2 from metabolic autoregulation.
14A14: Exam Report
Using a diagram, explain the effect of PaO2, PaCO2 and MAP (Mean Arterial Pressure) on cerebral blood flow (CBF). (60 % of marks) Outline the effects of propofol and ketamine on CBF and cerebral metabolic requirement for oxygen (CMRO2). (40% of marks)
74% of candidates passed this question.
This question was well answered. It is a structured question that guides candidates through exactly what is required. Well drawn graphs were a particularly effective means of scoring marks.
G4iii / K1iii / 23B14 / 21A20 / 14A14: Using a diagram, explain the effect of PaO2, PaCO2 and MAP on CBF (60 marks). Outline the effects of propofol and ketamin on CBF and CMRO2 (40 marks)
Values
- CBF = 750mL/min (at rest) OR 50mL/100g/min → majority to grey matter which is more metabolically active
- 15% of CO
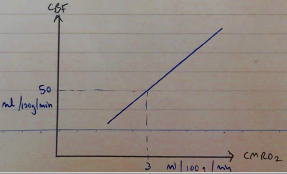
- CMRO2 is high = 3mL O2/min/100g
- This is 20% of total O2 consumption
- Brain is totally reliant on oxidative phosphorylation of glucose to provide ATP
∴ sensitive to hypoxia → high metabolic rate, no substrate stores
\( \textbf{CBF = } \frac{ \text{CEREBRAL PERFUSION PRESSURE} }{\text{CEREBRAL VASCULAR RESISTANCE}}\)
∴ Factors affecting CPP & CVR will determine CBF
CPP
CPP = MAP – (CVP or ICP)
(whichever is greater)
- MAP ~ 90mmHg
- ICP <13mmHg
∴CPP ~80mmHg
- NB: ICP is normally greater than CVP ∴CPP = MAP – ICP
- Any ∆ MAP & ICP will alter CPP
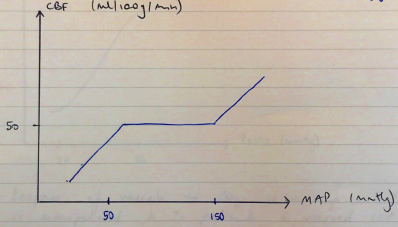
Note: CBF is kept constant b/w MAP 50 – 150mmHg*** by autoregulation
CVR
Pressure Autoregulation
- Constant CBF despite changes in MAP 50 – 150mmHg
- Myogenic Theory
- ↑P → ↑arterial wall stretch → VC → ↑minimal flow change
- R shift = chronic HTN
- L shift = neonates
- Impaired: volatiles, intracranial pathology
Cerebral Metabolism
- ∆ cerebral metabolism is met by ∆CBF
- Due to vasoactive metabolic mediators: H+, K+, adenosine, NO
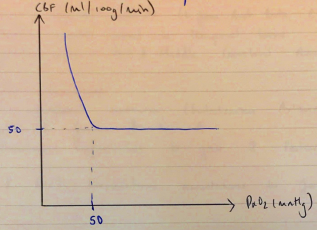
pCO2
- Linear relationship
- ↑PaCO2 1mmHg = ↑CBF 4% (between 20 – 80mmHg PaCO2)
- \( \text{This is low } CO_2 \text{ causes VD} \begin{cases} \text{CO2 diffuses across BBB} \\ \text{↑[H+]} \\ \text{Cerebral VD}\end{cases} \)
- Below PaCO2 20mmHg → VC → tissue hypoxia → build-up of metabolites → VD
NB: Response of vessels to CO2= is very important as it is manipulated to Tx patients with raised ICP
Nervous System
- Minimal change to CVR
- But very important to maintain CPP
- ↓BP → ↓BaroR firing → ↑symp activity → maintain CPP
Temperature
- ↓CMRO2 7% for each ↓1°C
- ↓CBF with ↓CMRO2
- Pyrexia/convulsions → ↑CMRO2 → ↑CBF
Drugs
↑CBF
Volatiles
Ketamine
↓CBF
PPF
Etomidate
Thiopentone
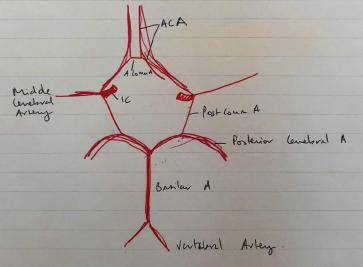
Anatomy of Cerebral Circulation
- Anterior & posterior circulation
Anterior Circulation
- Paired internal carotids (L from Arch Aorta, R from Brachiocephalic A)
- Enters carotid canal in temporal bone
- Divides into Ant & Middle Cerebral Arteries