K3i / 14A01: Motor + sensory pathways involved in withdrawal reflex
Outline the motor and sensory pathways involved in withdrawing the lower limb from a painful stimulus.
26% of candidates passed this question.
It was expected that candidates would outline both motor and sensory pathways and mention a reflex arc and conscious pathways.
Definitions
Reflex = involuntary and instantaneous movement in response to a stimulus
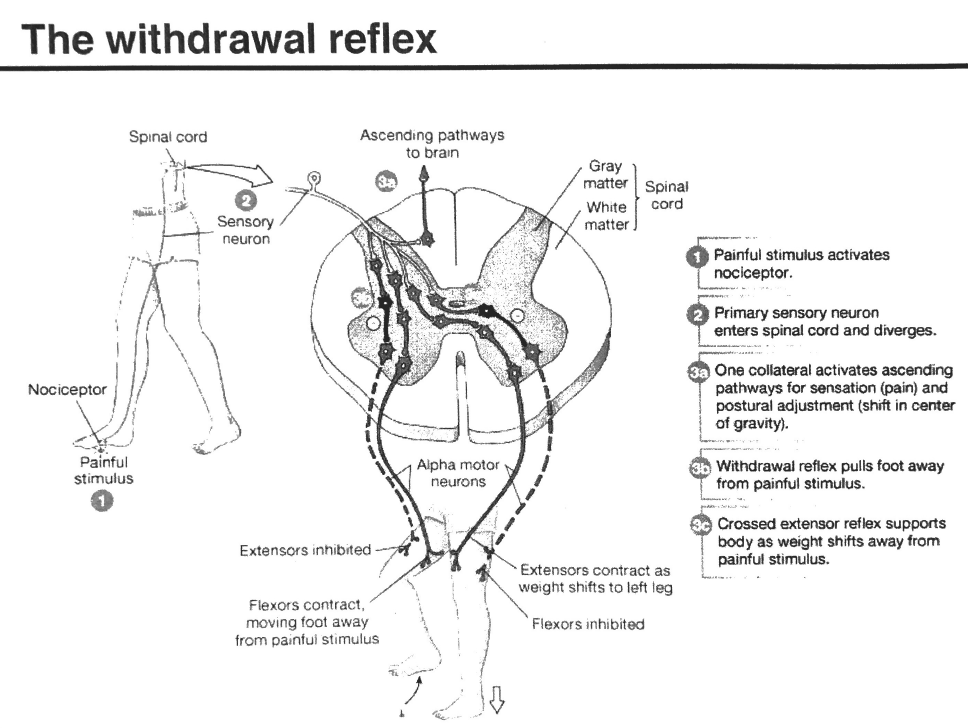
Withdrawal Reflex = A polysynaptic Reflex involving contact with a noxious stimulus resulting in flexion of limb in & inhibition of extensors in the same limb with simultaneous stabilisation of contralateral limb by extensor activation & flexor inhibition
Pain = an unpleasant sensory & emotional experience associated with actual/potential tissue damage
Physiology of pain involves:
- Peripheral detection
- Transmission (central + peripheral)
- Modulation
- Perception
- Reflex responses
Peripheral Detection
- Painful stimulus stimulates nociceptive aff n. fibres
- Aδ/C fibres (fast + slow pain)
- Release of NTs & neuropeptides by damaged tissue → K+, BK, leukotrienes, 5HT, histamine, Subs P
- Mediate inflammation + further nociceptive activation
Transmission
- Activated nociceptor with DRG cell body enters SC via Dorsal Horn
- Synapse with 2nd order neuron
- In Dorsal Horn Laminae II, I, V
- 2nd order neurons ascend in 2 tracts:
Spinothalamic (discriminates)
- Crosses ML
- Localises stimulus
- Type of pain
Spinoreticular (behavioural)
- Ascends ipsilateral to brainstem
- Integrates signals
- Emotional response
- 2nd order neurons synapse in THALAMIC NUCLEI with 3rd order neurons
- 3rd order neurons project through Internal Capsule to Cerebral (behavioural) + Somatosensory Cortex (discrimination)
Modulation
Peripheral sensitisation
- Tissue injury → NT/neuropeptide/inflammatory mediator release
- P4 synthesis → lowering of threshold to activate nociceptors
- ↑response to firing
- Activation of silent nociceptors
Central sensitisation
- Persistent stimulation of 2nd order neurons
- ↑ membrane excitability
- NMDA rec closely involved; ↑sensitivity to NTs
- Prolonged C-fibre input with ↑rate of firing for same stimulus or even after stimulus has stopped
Descending inhibitory pathways
- Originate in Somatosensory Cortex + Hypothalamus
- Activate Periaqueductal Grey Matter → disinhibits GABA neurons
- Activation of Nucleus Raphe Magnus → releases 5HT which activates inhibitory interneurons
- Both descend to Medulla + SC
- Inhibit asc. signals → provide analgesia
Perception
- 2nd order neurons travel in Neospinothalamic & Paleospinothalamic tracts
- Lateral spinothalamic tract → primarily responsible for transmitting to Somatosensory Cortex
- Type of pain, location of stimulus
Reflex Response
- Sensory neuron sends excitatory postsynaptic potential (EPSP) to somatic motor neuron originating in ventral horn
- EPSP makes postsynaptic neuron more likely to activate/depolarise
- 1° order neuron enters SC & diverges
- Somatic motor neuron exits ventral horn to activate motor neurons to flexor muscles → eliciting flexion + withdrawal of affected muscles (IPSILAT)
- Sensory neuron activates inhibitory interneuron
- Inhibits Motor neurons to extensor muscles via inhibitory interneurons (IPSILAT)
- Sensory neuron also activates an interneuron that decussates and crosses Midline of SC so that;
- Interneuron synapses and excites somatic motor n stimulating CONTRALAT extensor muscles
- Same interneuron inhibits flexors of CONTRALAT limb
∴ Withdrawal away from stimulus + crossed extensor reflex supports as body weight shifts (i.e. stepping on a pin)
- Author: Krisoula Zahariou