G4i / 18B16 / 16B19
18B16: Exam Report
Describe the forces that result in fluid exchange across capillary membranes.
57% of candidates passed this question.
The expected answer included a clear explanation of Starling’s forces, including an understanding of the importance of the relative difference along the length of the capillary, with approximate values and examples of factors that influence them. Some explanation of what contributed to the hydrostatic or osmotic pressure gained more marks than merely stating there
was a pressure. Several candidates digressed to Fick’s law of diffusion or intracellular flow of ions which was not directly relevant to capillary flow.
16B19: Exam Report
Describe how Starling forces determine fluid flux within the pulmonary capillary bed.
25% of candidates passed this question.
The equations for nett fluid flux and for nett filtration pressure were incorrect in many answers.
Better answers presented the equations and discussed each of the elements as relevant to the pulmonary capillary bed, including difference from systemic capillary beds.
Mention of the role of lymphatics and of the effect of surfactant, left atrial pressure, gravity and posture gained marks, also.
G4i / 18B16 / 16B19: Describe how Starling forces determine fluid flux within the pulmonary capillary bed Describe the forces that result in fluid exchange across capillary membranes
- Capillary wall is a SEMI-PERMEABLE MEMBRANE
- Permeable to H2O, solutes
- Impermeable to large proteins
- Produces a plasma ultrafiltrate
- Filtered by BULK FLOW through capillary wall by opposing hydrostatic + oncotic pressures
- The function of this bulk flow is the distribute fluid between intravascular & extravascular compartments → no nutritional benefit
Starling Forces
- Hydrostatic & oncotic pressures described by ∆ Starling Forces:
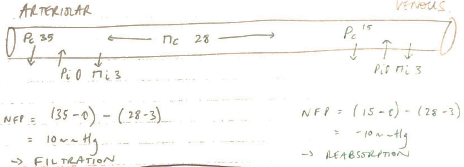
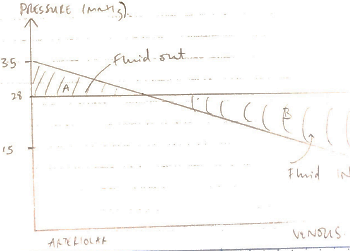
NET FILTRATION PRESSURE = Kf (PC – Pi) – σ (πC – πi)
Kf = Filtration Coefficient
- SA capillary walls x perm to H2O
- i.e. a ‘leaky’ capillary due to histamine will have high Kf
σ=Reflection Coefficient
- = Capillary permeability to proteins
- This value ranges from 0 – 1
- i.e. Hepatic sinusoids v. perm ~1
- CSF & glomerular v. low closer to 0
PC = Capillary Hydrostatic Pressure
- Pushes fluid into interstitial space
- Determined by arterial P, pre-cap & post-cap sphincter resistance
Pi = Interstitial Fluid Hydrostatic Pressure
- Pushes fluid into capillary
ΠC = Capillary Oncotic Pressure
- Generated by plasma albumin
- Generates an osmotic force
- Which prevents fluid moving out of capillary
- Stable at 28mmHg through vessel length
Πi = Interstitial Fluid Oncotic Pressure
- Generated by protein concentration of interstitial fluid
- Promotes fluid movement out of capillary
Fluid Loss
- NET FLUID LOSS from filtration is 4L/day
- This is all reabsorbed by lymphatics
- NOTE: some specialised capillaries can display filtration/reabsorption along the length of their vessels i.e.:
- Glom. Caps → always filter (huge hydrostatic pressures)
- Interstitial Caps → always reabsorb
Interstitial Oedema
- Occurs with accumulation of interstitial fluid
- Due to:
1. Imbalanced Starling Forces
- ↑PCg. fluid overload
- ↓πCg. malnutrition → ↓protein synthesis
- ↓Pig. negative pressure pulmonary oedema
- ↑πig. burns → plasma leak
2. Impaired Lymph Drainage
- Lymphoedema due to LN clearance or blockage i.e. infection
3. Kf ↑ / ↑ σ
- ↑Kf with infection/inflammation = leaky caps
- ↑σ in tissues with higher protein permeability i.e. liver
Consequences
- ↑diffusion distance for O2 & nutrients → this is very dangerous where there is a thin interstitial distance i.e. ALVEOLI
- Author: Krisoula Zahariou