F6iv / 18A03: Dead Space
18A03: Exam Report
Define dead space and its components (30% of marks). Explain how these may be measured (35% of marks) and describe the physiological impact of increased dead space (35% of marks).
59% of candidates passed this question.
Some candidates failed to provide a correct definition of dead space. An outline of anatomical, alveolar and physiological dead space was expected. The Bohr equation was commonly incorrect, and many did not comment on how to measure the components of the Bohr equation. Fowler’s method was generally well described though some plotted the axes incorrectly.
The impact of increased dead space was not often well explained. Very few people stated the major impact of increased dead space is reduced minute ventilation and how this would affect CO2.
F6iv / 18A03: Define dead space and its components (30% of marks). Explain how these may be measured (35% of marks) and describe the physiological impact of increased dead space (35% of marks).
Definitions
- Dead Space = VT that does not partake in gas exchange
- V/Q = ∞
- Alveolar ventilation = the effective part of VT that takes part in gas exchange
VA (alveolar ventilation) = RR (VT – VD)
Types of Dead Space
- Apparatus
- Anatomical
- Alveolar
- Physiological (anatomical + alveolar)
Apparatus Dead Space
- Due to artificial breathing apparatus
- Anaes. Circuit, HME filter, ETT
Anatomical Dead Space
- The volume of conducting airways
- 150mL
- Measured by Fowler’s Method (N2 washout)
- Influenced by:
- Age = ↑ with ↑age & infancy
- Posture = 150mL sitting, 100mL supine
- Neck position = ↓with flexion, ↑with extension
- Drugs = ↑with bronchodilators
- VT = ↑VT = ↑ because of traction on airways with large inspiration
Measured by Fowler’s method
- Subject breathes through valve box
- Sampling tube with rapid N2 analyser at lips
- Single FiO20 inspiration
- Breathes out through mouth piece
- 2 graphs
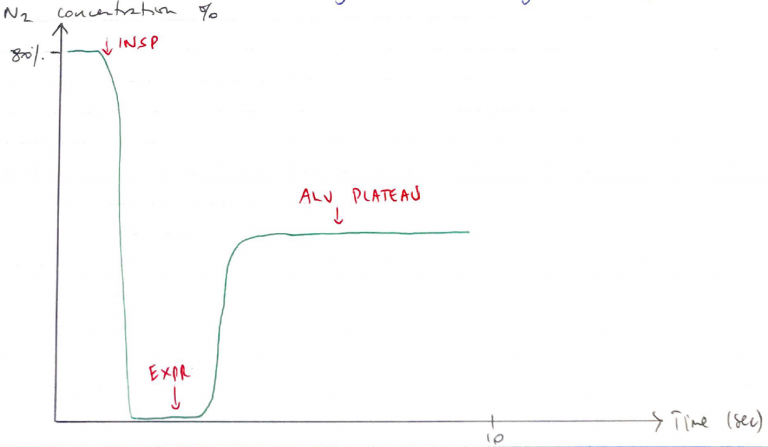
[N2] vs Time
- 3 phases
- Start of expiration, no N2 because it’s measuring expired gas of conducting airways (FiO20)
- N2 starts rising, because gas from alveoli starts mixing with gas from airways
- Plateau → only alveolar gas being recorded
[N2] vs Expired Volume
- Plot [N2] against expired volume
- Draw vertical line in S so that A = B
- DS is volume up to the vertical line
Alveolar Dead Space
- Volume of gas reaching alveoli that doesn’t take part in gas exchange
- WZ1 (PA > Pa > PV) i.e. IPPV or PE
- VQ = ∞
- This is pathological
- Normally ~5mL
- Measured by subtracting anatomical from physiological DS
Alveolar DS = Physiological – Anatomical
Physiological Dead Space
- VT which does not take part in gas exchange
Physiological DS = Alveolar DS + anatomical DS
- Influenced by:
- Age = ↑ with ↑age
- Sex = ↑with men
- Posture = ↑with supine
- Lung volume = ↑VT = ↑ because of traction
- Pathology = PE, smoking, IPPV
- Measured using BOHR EQUATION
- Underlying principle that expired CO2 comes from alveolar gas, not DS units
- It gives you the volume of VT that does not eliminate CO2
- In health the volume derived from Bohr’s & Fowler’s methods should be similar
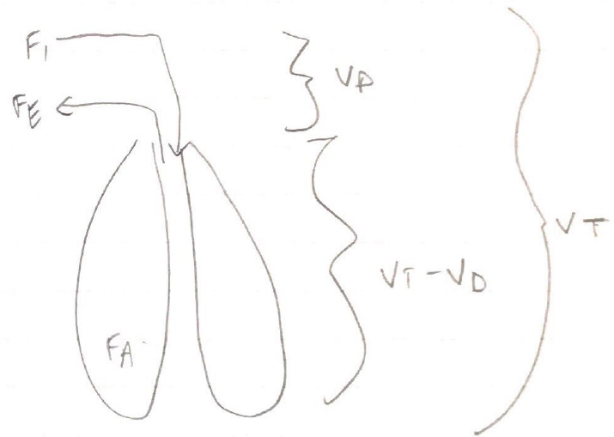
Exhaled VT = Alveolar Volume + DS Volume
- Analysed for any gas i.e. CO2
- Fe = expired CO2
- FA = expired alveolar CO2
Causes of ↑ Dead Space
- Hypotension
- PE
- Artificial ventilation → preferentially pushes air to upper lung & ↑PA
- Local vessel destruction
Consequences
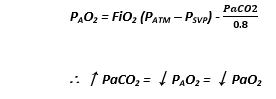
- Dead space produces hypercarbia & hypoxia
- Your PaCO2 will rise & your ETCO2 will fall (because remember, you’re not getting gas exchange so ↑CO2 in body + less being expired)
- Normal PaCO2 – ETCO2 is 1 – 5mmHg
- Hypercarbia = PaCO2 > 45mmHg
- Effects on 4 main system:
1. Intracellular
- CO2 small & soluble
- Crosses PM → depresses cellular metabolism 2° acidosis
2. Neurological
- Stimulates central & peripheral ChemoR to ↑MV
- ↑WoB
- ↑Symp stimulation → ↑HR & VC
3. Cardiovascular
- VD → flushing
- ↑CO
- Negative inotropy
- ↑risk of arrythmias 2° ↑H+ & ↓O2
- Author: Krisoula Zahariou
![[N2] vs Expired Volume](https://jennysjamjar.com.au/wp-content/uploads/2020/05/N2-vs-Expired-Volume-768x433.png)