F12i / 18A08: Outline the principle of co-oximetry (40 marks) + describe what a co-oximeter is able to measure (30 marks) + Compare its limitations to those of a pulse oximeter (30 marks)
18A08: Exam Report
Outline the principle of co-oximetry (40% of marks), describe what a co-oximeter is able to measure (30% of marks), and compare its limitations to those of a pulse oximeter (30% of marks).
32% of candidates passed this question.
Most candidates confused co-oximetry with other methods of measuring oxygenation of blood. Whilst there were a number of excellent descriptions of pulse oximetry, these attracted no marks for the first two sections. Structuring the answer based on the three parts asked, would have improved answers ensuring all aspects of the question were addressed.
F12i / 18A08: Outline the principle of co-oximetry (40 marks) + describe what a co-oximeter is able to measure (30 marks) + Compare its limitations to those of a pulse oximeter (30 marks)
Definition
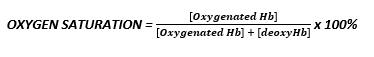
A co-oximeter is a spectrophotometer designed to measure blood oxygen saturation, taking into account numerous Hb species of blood
Principle
- Consists of:
- Haemolyser unit
- Photo lamp
- Lens system
- Sensing photodiodes
- Small sample of blood is heparinised & injected into co-oximeter
- Sample heated to 37°C & haemolysed by vibrations
- Haemolysed solution gives translucent solution
- Incompletely haemolysed RBC can scatter light & introduce error
- Light from lamp is filtered & focused to pass through blood sample
- Up to 17 wavelengths produced by filter wheel
- Result available in 30 secs
- Each of the haemoglobins has a unique absorption spectrum
- ∴uses BEER-LAMBERT LAW to measure absorption
BL Law = Light transmitted through a substance ↓ exponentially with ↑ distance & concentration
Measured Indices
- SaO2
- Total Hb
- O2 content
- Met Hb %
- Sulpha Hb %
- CO Hb %
NB → some can distinguish foetal Hb
Importance
- Each Hb (deoxyHb, oxyHb, COHb, MetHb) has its own light absorption
- Pulse ox only uses 2 wavelengths → assumes that blood contains only OxyHb + deoxyHb
- ∴ Pulse ox can give misleading SpO2 in presence of dysglobinaemias
- Co-oximetry important when:
- Hx toxin exposure
- Hypoxia fails to improve with ↑FiO2
- Discrepancy b/w SpO2 & PaO2
- Suspicion of abnormal Hb
Compared to Pulse Oximeter
Pulse Ox
Non-invasive
Co-Oximetry
Invasive
- Requires blood sample
- Although new pulse co-ox is becoming available with ability to measure 8 wavelengths
Pulse Ox
Transportable easily
No calibration but error +/- 3 of SpO2
70 – 100%
Co-Oximetry
Heavy machinery + requires calibration
Pulse Ox
SENSOR
- Requires adequate light transmission
- Can be interrupted by external light
- Uses red + IR
Co-Oximetry
SENSOR
- Sample injected into machine, but affected by external light/poor transmission
- Uses visible light only –> ∴ assesses Hb in plasma (not bone, skin, muscle etc)
Pulse Ox
ABNORMAL Hb
- Assumes blood only has Oxy & deoxyHb
- ∴doesn’t account for other Hbs
Co-Oximetry
ABNORMAL Hb
- Accounts for all Hb types & their absorption spectrum
- Low Co-Ox = TRUE HYPOXIA
Pulse Ox
BLOOD FLOW
- Affected by poor perfusion
- Confused by non-arterial pulsatile BF
Co-Oximetry
BLOOD FLOW
- Not affected by perfusion
Pulse Ox
TIME
- Continuous real time with lag
Co-Oximetry
TIME
- Fast answer but only gives SaO2 at time of sample
- Author: Krisoula Zahariou