G6ii / 18A18: Compare & contrast non-invasive oscillometric and invasive arterial blood pressure monitoring
18A18: Exam Report
Compare & contrast non-invasive oscillometric and invasive arterial blood pressure monitoring
52% of candidates passed this question.
There were some good answers, though invasive BP measurement was better answered than oscillometry. Many candidates provided extensive detail in one area i.e. the workings of a Wheatstone bridge, to the detriment of a balanced answer.
Few seemed to have a structure consisting of “equipment, method, sources of error, advantages, disadvantages” or similar and missed providing important information as a result.
Several described auscultatory non-invasive blood pressure measurement, rather than oscillometry, which although related in principle is a different process.
G6ii / 18A18: Compare & contrast non-invasive oscillometric and invasive arterial blood pressure monitoring
Non-Invasive Oscillometric
Invasive Arterial
Equipment
Monitor housing:
- Pump → to pressurise the system
- Valve → to depressurise the system
- Cuff
- Pressure transducer
- Microprocessor
- Display screen
- Gold Standard of BP measurement
Intra-arterial cannula
- Short, narrow, stiff so its resident frequency is outside harmonic range
- Teflon to ↓thrombus formation
- Narrow (20 – 22G) = risk of thrombus proportional to diameter
Fluid-filled tubing
- Column of non-compressible fluid for Hydraulic Coupling
- Short, fat, non-compliant tubing = ↓Damping
3-way tap
- Allows zeroing & blood sampling
Pressure transducer
- Consists of a diaphragm & a strain gauge
- Converts pressure waveform into electrical signal
Flush system
- Pressurised saline @300mmHg
- Allows slow infusion @ 2mL/hr to maintain patency
Signal processor cable
Electrical signal from transducer is transmitted for filtering, amplification, analysis & display on screen as Pressure v Time wave
Mechanism of Action
- Oscillation = periodic motion that repeats over time
- Oscillometric BP measurement measures oscillations caused by arterial pressure when blood flows through a heart that is restricted by a cuff
- Cuff applied to limb over an artery
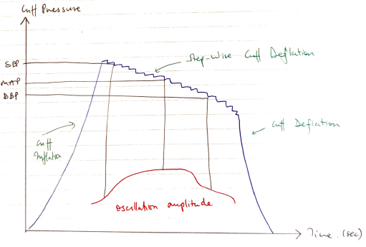
- Single cuff is automatically inflated to a predetermined level about SBP
- Cuff pressure continuously monitored by a pressure transducer in the machine
- Cuff is deflated in step-wise increments ~2mmHg/beat
- During each pressure hold, the pressure transducer measures whether pressure is constant or whether there are small regular oscillations
- Detecting:
- ONSET of rapidly increasing pulsations = SBP
- MAXIMUM pulsations = MAP
- ONSET of rapidly decreasing pulsations = DBP
- Frequency of oscillations = HR
∴MAP is the only variable directly measured → rest are estimated
Transducer = device that converts E. from one form to another
Strain Gauge = sensor whose electrical resistance varies with applied force
- Used to measure ∆pressure
- Arterial pulsation moves saline column back & forth
- Hydraulic Coupling causes diaphragm to move
- Flexible diaphragm attached to strain gauges
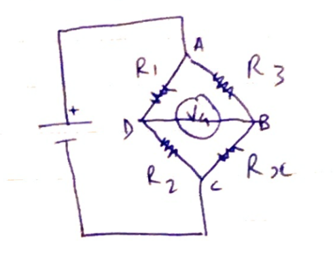
- All 4 strain gauges connected electrically to form Wheatstone Bridge circuit
3 resistors = known value
1 resistor = unknown (variable)
- Resistors are arranged so when R1/R2 = R3/Rx there is NO FLOW (null deflection)
The VG Galvanometer measures current flow between D & B
If the bridge is balanced, there is no flow
When diaphragm alters resistance in strain gauge, one gets stretched the other gets compressed (on the other side of the diaphragm)
Increased resistance is measured as change in current flow
Electrical signal transmitted via cable to microprosessor
Displayed as P v T wave
Sources of Error
- Cuff movement
- Rapid BP changes
- Arrhythmias
- Incorrect cuff size
- External cuff pressure
Static & Dynamic Calibration
Static calibration = ability to record stationary event
- Requires zeroing
- Zero reference point is the air-fluid interface above/below diaphragm when tap open to air
- Zero reference pt & cannula tip need to be the same level → ∴each time patient is moved the transducer height should be moved/system re-zeroed
Dynamic calibration = reliably record rapidly changing events
Resonant frequency = the frequency at which the system oscillates when disturbed
→ The NF of the IABP should be much higher than the primary of the waveform
→ Otherwise the system will resonate excessively
→ Overestimate SBP, underestimate DBP
Damping = the absorption of the Energy of oscillations which will ↓ their amplitude
→ Damping caused by
- Friction in fluid pathway
- Vasospasm
- 3-way taps
- Narrow, long, compliant tubing
- Kinks in cannula/tubing
Advantages
- Convenient
- Reasonable accuracy
- Continuous measurement
- Sensitive
- ABGs
- Waveform analysis
- Pulse pressure variation
- Direct measurement of all pressures (SBP, DBP, MAP) & HR
Disadvantages
- MAP is the only reliable measurement
- Ulnar nerve injury
- Petechiae haemorrhage under cuff inflation site
- Expensive
- Single use
- Less portable
- Delicate
- Requires expertise
- Bleeding, infection, thrombosis, tissue damage
- Author: Krisoula Zahariou