K2ii / 18B19: Describe toxicity of local anaesthetic agents
18B19: Exam Report
Describe toxicity of local anaesthetic agents.
28% of candidates passed this question.
Most questions lacked a systematic approach to the question and specific detail. The relationship between systemic toxicity (CNS and CVS) and plasma levels should be described. Many candidates did not clearly state that CNS toxicity occurs at lower plasma levels that CVS toxicity. Factors that affect toxicity (e.g. drug factors, patient factors, interactions) needed to be
elaborated with some detail. Patient factors such as age, pregnancy, acidosis, hyperkalaemia, hepatic failure were often omitted. Finally, marks were also awarded for noting methaemoglobinaemia as possible toxicity and the existence of specific therapy (intralipid).
K2ii / 18B19: Describe toxicity of local anaesthetic agents
Definitions
Toxicity = occurs when the physiological response to a drug is an adverse effect
Classification of LA Toxicity
- Systemic Toxicity
- Local Neurotoxicity
- Hypersensitivity Reactions
- Agent Specific Toxicity
a. MetHb w Prilocaine
b. Cocaine toxicity
Systemic Toxicity
Excess plasma concentration of a drug due to absorption and distribution of drug distant to its entry point
- The most common adverse reaction to LAs is systemic toxicity
- Usually due to accidental IV injection / overdosage
- PPB sites become quickly saturated and unbound drug is available to diffuse into CNS & conducting tissue of heart
- Symptoms of LA toxicity correlate well with plasma levels:
Plasma Lignocaine
Symptoms
4mcg/ml
Lightheaded, Dizzy, circumoral/tongue paraesthesia
6mcg/ml
Visual disturbance, nystagmus, tinnitus
8mcg/ml
Slurry speech, muscle twitching
CC/CNS RATIO
\( \textbf{CC/CNS Ratio = } \frac{\text{Blood level for cardiovascular}}{\text{Blood level for convulsions}} \)
- CC/CNS Ratio = the ratio of blood levels required to produce irreversible cardiovascular collapse cf the blood levels required to produce convulsions
- CC/CNS Lignocaine = 7
- CC/CNS Bupi = 2.7
- Therefore, x7 much as much drug will induce irreversible CVS collapse cf the dose required to produce convulsions, thereby providing enough warning of toxicity before CVS collapse
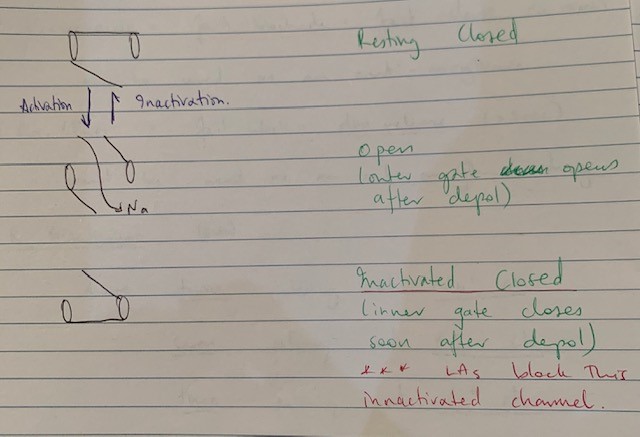
CNS Toxicity
- 2 stage process:
- Blocking Na ch of inhibitory neurons = unopposed excitation = convuslsions
- Total neuronal blockade = CNS depression
- Slowing/silent EEG
- Coma
- CVS collapse
- 2 stage process:
CVS Toxicity
Direct
- Negative inotropy
- Delayed conduction
Indirect
- Autonomic outflow block
- CVS centre of midbrain depression
- Results in HTN & tachycardia secondary to CNS excitation
- Then myocardial depression and ↓CO → peripheral VD & severe ↓BP → brady/dysrhythmia → Cardiovascular collapse
Factors which Increase the Risk of Toxicity
Ceutic
- R enantiomer;
- Racemic (Bupi) mixtures
- Twice as potent at Na channels
- Seven times as potent at K channels
- Three times as potent at Ca channels
- Racemic (Bupi) mixtures
PK
A
Diffusion from site of injection obeys Fick’s Law:
\( \textbf{Rate of Diffusion = } \frac{\text{SA}}{\text{T}} \textbf{ x } \frac{\text{Solubility}}{\sqrt{\text{MW}}} \textbf{ x } (C_2 – C_1) \)
- Dose: ↑dose = ↑ rate of diffusion
- Max doses:
Drug
Maximum Dose
Adrenaline – can be added to LAs for its potent VC properties ↓rate of absorption and therefore ↓rate of rise of plasma levels. But, it carries its own risk of arrythmias & tachycardia
Drug
Cocaine
Maximum Dose
1.5-2.0mg/kg (independent of adrenaline) to maximum of 100mg
Drug
Prilocaine
Maximum Dose
8mg/kg (plain) to maximum of 400mg
10mg/kg (+Adr) to maximum 600mg
Drug
Lignocaine
Maximum Dose
3-5mg/kg (plain) to maximum dose of 200mg
7mg/kg (+ adrenaline) to maximum of 500mg
Drug
Bupivacaine
Maximum Dose
2mg/kg (independent of adrenaline) to maximum of 150mg
Drug
Ropivacaine
Maximum Dose
<3mg/kg (independent of Adr) to maximum 200mg
- Injection site: ↑degree of vascularity = ↑plasma concentration; IC > Epidural > subcutaneous
D
- Lipid solubility: ↑lipid solubility = ↑potency (Bupi > Ropi > Lignocaine)
- pKa: the closer to physiological = ↑ [UNIONISED] = ↑speed of onset
Lig 25% > Bupi 15% > Ropi 14% unionised at pH 7.4
- PPB: plasma proteins quickly become saturated = ↑%free drug = ↑toxicity, therefore, any condition ↓plasma proteins = ↑risk toxicity
M
- Amide LAs metabolised by N-dealkylation and hydrolysis in liver
- ↓metabolism (liver failure) = ↑availability of drug in plasma =↑risk toxicity
E
- 10% excreted unchanged by kidneys
- ↓renal fn = ↓renal excretion = ↑half life & risk of toxicity
PD
- CC:CNS Ration: measure of safety, drug w ↓ratio = ↑risk toxicity
Lignocaine 7 > Ropi 5 > Bupi 3
- Inter-individual variation: sensitivity of Na and Ca channels
- Acidosis: fetus, shocked states = ↑ionised portion & ion trapping of LA = ↑risk toxicity
- ↑PaCO2 = acidosis + ↑CBF = ↑delivery to CNS =↑risk toxicity
- ↑K = ↓RMP = facilitates depolarisation = ↑risk toxicity
Treatment of systemic toxicity (although not asked for, awarded points!)
- Stop injection + get more IV access
- FiO2 100% + intubate to avoid hypoxia
- ↑MV (acidosis = ↑ionised form)
- Elevate legs, vasopressors to maintain CO
- Control seizures (benzos)
- Lipid emulsion Tx
- CC = ACLS protocol
Local Neurotoxicity
- Histiotoxicity from LA preparation
- Direct trauma from needle
- Trauma from positioning
- Range of neurological injury from patchy numbness → cauda equina syndrome
Hypersensitivity
- <1% of adverse reactions to LAs are due to an allergic mechanism
- Genuine hypersensitivity to additives Methylparaben, Metabiusulphate
Agent Specific
Cocaine:
- Myocardial ischaemia due to CA vasospasm and sympathetic stimulation
- Reduced uterine BF and foetal hypoxaemia
- Hyperpyrexia
- CVAs
Prilocaine – Methaemoglobinaemia
- Author: Krisoula Zahariou