F6ii / 21B10: Describe the ventilation / perfusion (V/Q) relationships in the upright lung according to West’s zones (40%). Explain the physiological mechanisms responsible for these relationships (60%).
21B10: Exam Report
Describe the ventilation / perfusion (V/Q) relationships in the upright lung according to West’s zones (40%). Explain the physiological mechanisms responsible for these relationships (60%)
47% of candidates passed this question.
This is a core aspect of respiratory physiology, and a detailed understanding of this topic is crucial to the daily practise of intensive care. As such the answers were expected to be detailed. Strong answers included precise descriptions of the zones of the lung as described by West and related these to the V/Q relationship in the upright lung. Generally, most candidates scored well in this section. Diagrams were of varying value. However, an impression from the examiners was that candidates spent too much time on this first section and ran out of time for a detailed answer in the second section. The answers to the second section seemed rushed and were often lacking in detail with many incorrect facts. This question highlights the importance of exam technique preparation in the lead up to the written paper.
F6ii / 21B10: Describe the ventilation / perfusion (V/Q) relationships in the upright lung according to West’s zones (40%). Explain the physiological mechanisms responsible for these relationships (60%).
West’s Zones
Definition
West Zones describe the regional blood flow through the lungs – blood flow is analogous to a Starling resistor, where the driving force for blood flow is the difference between pulmonary arterial and venous pressure, and the resistive force is the alveolar pressure.
West described these zones using constant blood flow (i.e. not pulsatile), and at static lung volumes/pressures (i.e. does not account for the respiratory cycle).
Zone 1
Alveolar Pressure (PA) > Pulmonary Arterial Pressure (Pa) > Pulmonary Venous Pressure (Pv)
- There is no (or practically no) blood flow in Zone 1 as alveolar pressure exceeds arterial pressure and the blood vessels collapse
- This produces a V/Q ratio of infinity (dead space)
- This should not occur in healthy, spontaneously breathing people
- May occur when:
- Low pulmonary artery pressures (e.g. hypovolaemic shock)
- High alveolar pressures (e.g. positive pressure ventilation with high PEEP)
Zone 2
Pa > PA > Pv
- The rate of blood flow is determined by the difference between Pa and PA
- Blood flow increases linearly from the upper parts of the zone to the lower parts of the zone as Pa increases with gravity.
- The V/Q ratio in the upper parts of Zone 2 is ~3 and increases in the lower parts
- Zone 2 is the majority of the lung in normal conditions
Zone 3
Pa > Pv > PA
- The rate of blood flow is determined by the difference between Pa and Pv
- Blood flow is highest in this region
- Blood flow continues to increase in the lower parts of this zone as small vessels can be distended -> reduces resistance to flow
- The V/Q ratio in the lower parts of Zone 3 approaches 0.3
Zone 4
Pa > Interstitial Pressure (Pi) > Pv
- Described later than the first 3 zones
- Blood flow is determined by the gradient between Pa and Interstitial pressure
- Occurs in atelectatic or oedematous lungs at the very bases
Regional V/Q Relationships
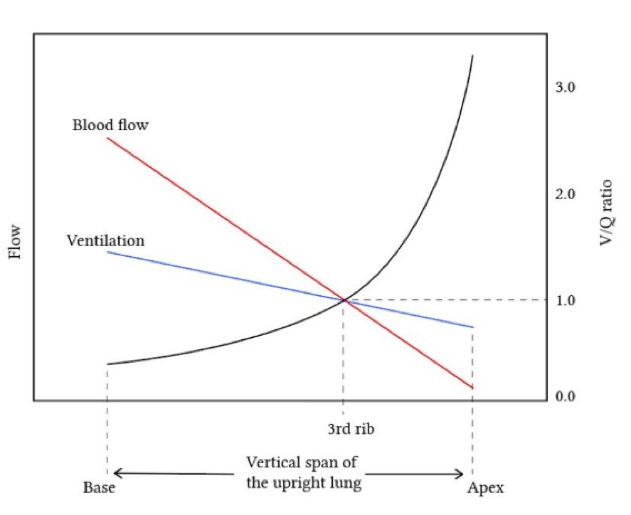
- Blood flow (i.e. perfusion) increases from the apex to the base
- Ventilation also increases from the apex to the base, but to a lesser degree
- The V/Q ratio therefore decreases from ~3 at the apices to ~0.3 at the bases.
Mechanisms Responsible For V/Q Relationships
Factors that influence perfusion:
The balance between hydrostatic pressure of blood and alveolar pressure -> behaves like a Starling resistor
- Collapse of blood vessels in Zone 1
- Distension of blood vessels in Zone 3
Hydrostatic pressure of blood
- Gravity and posture
- The effect of gravity reduces the hydrostatic pressure at the apices, and increases it at the bases
- Changes in posture alter the distance in which gravity acts – blood flow is equal between the apex and base in the supine position (but the anterior lungs get less blood flow than the posterior)
- Increased pulmonary artery pressure – e.g. Exercise, L->R intra-cardiac shunt
- Results in increased blood flow (as long as the cause does not similarly increase PA or Pv)
- Increased pulmonary venous pressure – e.g. LV failure, mitral stenosis
- Results in more Zone 3 (Pv > PA) and blood flow becomes more uniform throughout the lungs. Total blood flow may increase or fall, depending on the change in Pa
- Hypoxic pulmonary vasoconstriction
- The pulmonary vasculature alters it’s resistance regionally to direct blood away from poorly ventilated, hypoxic regions of the lung. This improves V/Q matching.
Alveolar pressure
- Constant throughout the lung (despite a vertical pleural pressure gradient)
- Therefore, the West zones depend primarily on changes in hydrostatic pressure throughout the lung
- Positive pressure ventilation (PPV)
- Increases alveolar pressure – PEEP is the main determinant. Higher pressures result in more Zone 1, Zone 2 extends further down the lung
- Gas trapping (e.g. asthma)
- Similar to PPV, although the increased pressure is due to incomplete expiration and dynamic hyperinflation
Other mechanisms affecting pulmonary blood flow
The pulsatile nature of blood flow and the respiratory cycle
- Blood flow changes throughout the cardiac cycle – highest in systole, lowest at end-diastole
- PA changes throughout the respiratory cycle (lower in inspiration, higher in expiration)
- This results in the borders of West Zones moving within the lungs in normal physiology.
Factors that influence regional ventilation:
- Vertical pleural pressure gradient
- The effect of gravity means that the pleural pressure is more negative at the apex than the base
- This results in the apical alveoli being more distended -> less capacity to distend on inspiration -> less well ventilated than the bases
- Lung compliance
- The lung bases are more compliant -> more ventilated
- Decreased in global compliance (e.g. high or low lung volume, ARDS) will result in decreased global ventilation -> lower V/Q ratio
- Anatomical expansion potential
- The anatomy of the lower part of the chest and the diaphragm mean that the bases have more space to expand in inspiration -> contributes to improved ventilation
- Pattern of breathing (diaphragmatic vs chest wall/accessory muscles)
- Diaphragmatic breathing (normal) expands the bases more than other regions of the lung
- Accessory muscle use contributes to increased expansion of the apices and mid-zones of the lungs
Author: Joshua Mclarty