Q1iv / 21B19: Outline the process of fibrinolysis (40% marks). Write short notes on the indications, mechanism of action, pharmacokinetics and side effects of tranexamic acid (60% marks)
21B19: Exam Report
Outline the process of fibrinolysis (40% marks). Write short notes on the indications, mechanism of action, pharmacokinetics and side effects of tranexamic acid (60% marks)
30% of candidates passed this question.
The relative allocation of marks and thus time to be spent on each component was delineated by the relative percentages in the question. The first part of the question required a step-by-step outline of the fibrinolytic pathway with mention of the regulatory processes. Tranexamic acid is an important drug in the practice of intensive care and the question provided the headings under which to answer the question. The detail surrounding the keys aspects of this drug with respect to its use in critical care were often vague and underappreciated.
Q1iv / 15B19: Outline the process of fibrinolysis (40% marks). Write short notes on the indications, mechanism of action, pharmacokinetics and side effects of tranexamic acid (60% marks)
Definition
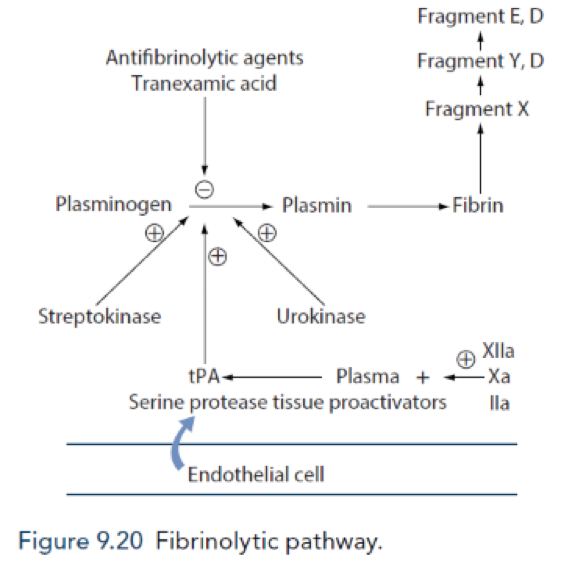
- Plasminogen is a β-globulin (proenzyme synthesised by liver)
- Plasminogen becomes interwoven into fibrin clot as it is formed
- Plasminogen \( \underrightarrow {\text{tPA (expressed by endothelial cells) }} \) plasmin (serum protease)
- Keeps endothelial cell surface free of fibrin deposits → small vessels patent
- Fibrin is cleaved by plasmin → fibrin degradation products (FDP)
- D-dimer (a FDP): cleavage product of cross-linked fibrin
- Much slower process than coagulation
- Time lag between clot formation & clot dissolution allows healing to take place
- Extrinsic activation (from the tissues) → by endothelial tPA (enhanced by local thrombin production), which circulates and activates ONLY fibrin-bound plasminogen (ie localised to the clot)
- Intrinsic activation (from the vessel wall) → by CF XIIa, kalikrein
- Urokinase → produced by monocytes, macrophages, urinary epithelium
Regulatory processes
Mechanism of Action
Increases Fibrinolysis
Decreases Fibrinolysis
Mechanism of Action
Effect on plasmin
Increases Fibrinolysis
Decreases Fibrinolysis
Plasmin inactivation:
- Α2 macroglobulin
- Α2 antiplasmin
Mechanism of Action
Effect on plasminogen
Increases Fibrinolysis
Facilitate the conversion of plasminogen to plasmin
- Streptokinase
- Urokinase
- Tissue plasminogen activator
- Alteplase
Decreases Fibrinolysis
Competitively inhibits the conversion of plasminogen to plasmin
- Tranexamic acid
Regulation of Fibrinolysis
- Plasmin Activator Inhibitor (PAI) 1 & 2: produced by vascular endothelium and inhibits tissue plasminogen activator and urokinase
- Protein C inactivates plasmin activator inhibitor, thrombin activatable fibrinolysis inhibitor
- Thrombomodulin (expressed on intact endothelium): binds thrombin and subsequently activates protein C
- Thrombin activatable fibrinolysis inhibitor: produced by liver & cleaves plasmin binding sites on fibrin → ↓degradation
- α2 antiplasmin: produced by liver, inhibits circulating plasmin, not fibrin bound plasmin
Tranexamic acid
Tranexamic Acid
Chemical
A synthetic analogue of LYSINE
WHO’s list of essential medicines
(the most effective & safe medicines needed in a health system)
Use
- Cardiac sx (↓peri-op bleeding)
- Reverse thrombolytic therapy
- Menorrhagia
- Dental bleeding
- Epistaxis
- Haemoptysis
- Haemorrhagic shock (Trauma, Obs + surgical haemorrhage)
- DIC
Presentation
Tablets 500mg
Vials
- 5000mg/50mL
- 1000mg/10mL
- 500mg/5mL
Dose
Menorrhagia: PO 1g QID
IV 20mg/kg over 5 mins
Trauma/haemorrhage: IV 1g over 10min (IV) → 1g IV over 8hrs
Epistaxis → topical
Mouthwash → 10mL 5%
Dose adjust in ↓renal impairment
Route
PO/IV
Onset
5 – 15 mins → DoA 3hrs
MoA (mechanism)
- Binds plasminogen lysine binding sites (REVERSIBLE)
- Competitively inhibits activation of plasminogen → plasmin
- ∴stops fibrinolysis
- 10 x stronger than aminocaproeic acid
- At v. high doses inhibits PLASMIN
PD
(systems)s
PK
A
OBA 34%
D
3% PPB because binds almost exclusively to plasminogen
M
Minimal
E
Urine
95% unchanged
t ½ 2 – 11hrs
Adverse Effects
Ocular – vision ∆
Seizures
Renal impairment
Pulmonary Hypertension
Hypotension with rapid administration
GI disturbance (PO) → N&V, diarrhoea, GORD
Intravascular thrombosis (largely theoretical); no consistent data that shows increased risk of thrombosis with its use
- Discovered by Utako Okamoto in 1950s
… who was looking for a drug to treat PPH
- She could not persuade Kobe obstetricians to use it… however eventually made its way to the WHO essential medicine list!
Author: Novia Tan